
Eating. Drinking. Breathing. The genesis of all these critical functions lies in our mouth: the veritable gateway to our body. Yet in the broader picture of whole body wellbeing, we rarely consider the critical role of oral health.
This tragic alienation is due, in part, to the healthcare industry’s separation of dentistry from the rest of the medical world. Dental insurance, for example, differs from medical insurance. Dental checkups, while considered routine annual norms, are arguably less emphasized than visits to the doctor. Societal emphasis falls on aesthetic and external appearance of our smiles, with an explosion of teeth whitening products, veneers, and cosmetic dentistry, rather than the health of our teeth and gums.
While we are accustomed to believe the foundation of oral health involves X-rays for cavities and physical evaluations of gum disease, the true key to personalized, prevention-focused, and evidence-based medicine for oral health, and addressing the root cause of oral disease may be found in a different frontier: the oral microbiome.
Like its precedence in practice – the ever increasing exploration of the gut microbiome - we now bear the ability to analyze the environment of our mouths at the microbial level. While this concept was on my radar for awhile, I was thrilled to meet Bristle, a company which created a first-of-its-kind, at home, comprehensive oral microbiome test to help measure, understand, and improve oral health. Our oral microbiome controls our risk for oral diseases and impacts our overall health, and everyone’s oral microbiome is different. With Bristle, we can understand our unique oral microbiome and how it impacts our disease risk, take steps to improve our oral health, and ultimately monitor progression over time.
The Oral Microbiome
Our bodies are awash in an array of microbiomes: gut, skin, mouth, and genital. Even an invisible microbiome cloud surrounds out bodies! (Think Pig Pen in Charlie Brown, for better or worse.) The largest of these microbiomes, the gut microbiome, came into the spotlight over the last decade, and holds clues to many aspects of our overall health: everything from gut disorders, to mental health, to autoimmune conditions, to risks for certain types of cancer.
Following the gut, our mouth is actually our second largest, diverse microbial community, composed of bacteria, fungi, and viruses. An individual’s unique oral mosaic features trillions of microbes, from 100 - 200 species (out of 700 potential species) residing in the oral cavity, which encompasses our tongue, cheeks, teeth, and every little crevice in between. These microorganisms exist as free-swimming planktonic cells, or assemble together to form a biofilm: a complex structure of microbes which attach to a surface like a tooth, and manifest as plaque or dental calculus.
Our mouths are a delicate balance between these good and bad bacteria. In the warzone of our mouth, beneficial microbes are crucial to keeping us healthy, while harmful microbes directly cause diseases, including cavities and gum disease. When dysbiosis occurs, the delicate balance is tipped, and the bad start outnumbering the good. In such a state, we become more susceptible to complications like cavities, tooth loss, gum disease, and bad breath.
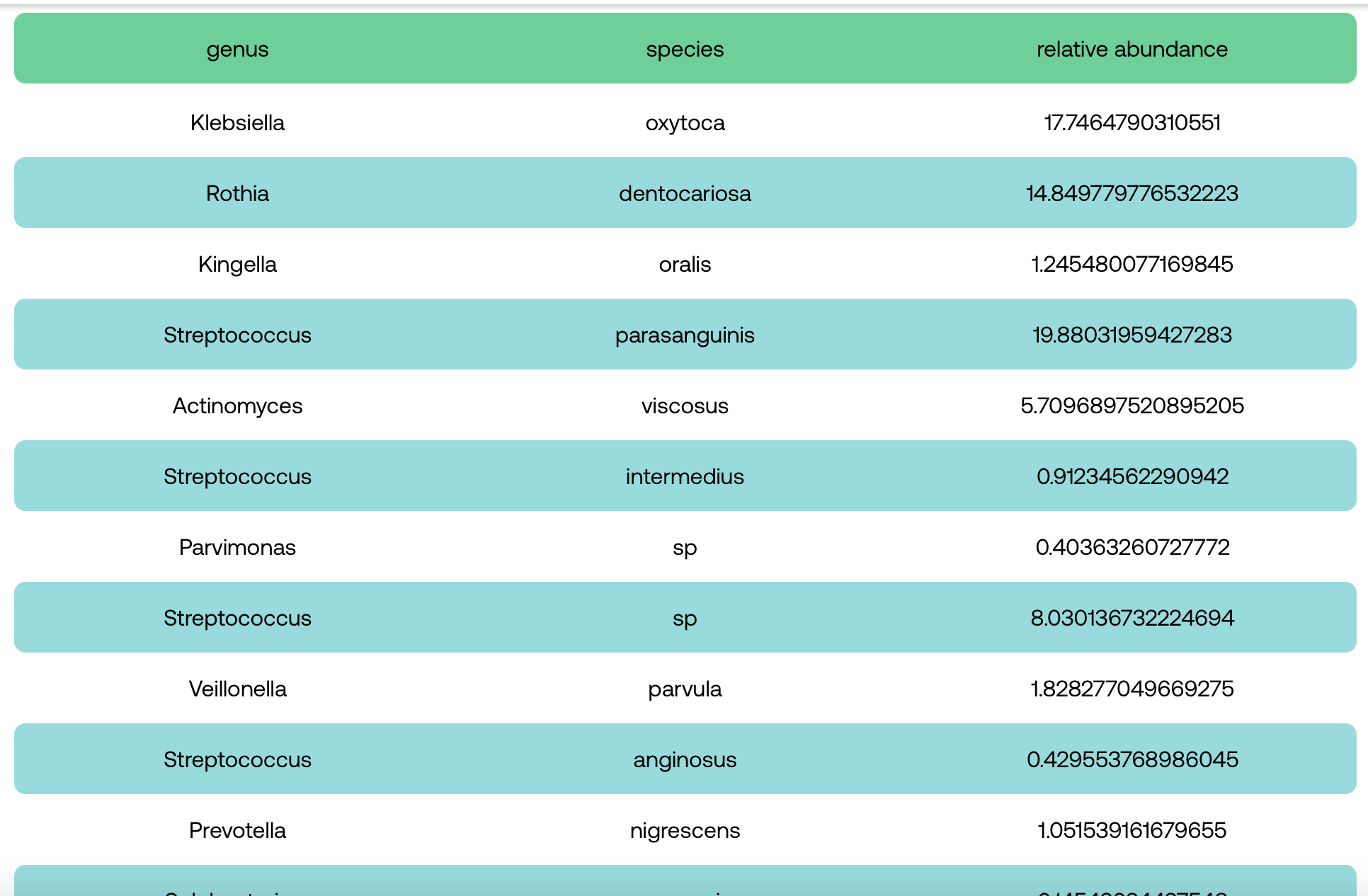
Some bacteria from the raw data from my Bristle results! Get 15% off Bristle with the code melanieavalon at melanieavalon.com/bristle.
Beneficial Bacteria And The Problems With Oral Care Products
The beneficial bacteria of our oral microbiome serve as heroic microbial buddies playing a critical role in keeping us functioning at our best. These bacteria typically thrive in a neutral or high pH environment, including the likes of Lactobacillus reuteri, Neisseria mucosa, and Streptococcus sanguinis.
Digesting food begins in our mouth, where certain beneficial bacteria help break apart proteins and sugars, and stimulate saliva, one of our body's natural healers and cleansers. Saliva washes away food which might otherwise serve to feed harmful bacteria, and also covers our teeth, acting as a defensive barrier. Furthermore, saliva contains calcium, fluoride, and other minerals that help repair the protective surface of our teeth through a process called demineralization.
Bacteria in our mouths also help facilitate denitrification, a critical process to our overall health. Found in many of the foods we eat, the chemical compound nitrate is particularly abundant in vegetables and fruits, such as beets and leafy greens. Certain oral bacteria reduce nitrate to nitric oxide, a molecule in our body that powers vasodilation: the dilation of blood vessel which is essential for reducing blood pressure, promoting metabolic and cardiovascular regulation, and improving cognitive function.
While various oral care products boast killing 99.9% of bacteria, such an approach is severely shortsighted. Antimicrobials often wipe out not only the harmful bacteria, but also the commensal and probiotic species which are necessary to achieve better health.
ORAL HEALTH ISSUES
Tooth Decay And Cavities
With every hero comes a villain, and the oral microbiome is no exception. Specific problematic bacteria drive tooth decay and cavities, which are actually the most prevalent chronic diseases on the planet in both children and adults.
Certain species of oral bacteria – such as the primary player Streptococcus mutans – convert sugar from the foods and drinks we consume into acid. An acidic oral environment encourages the buildup of biofilm into plaque: a sticky bacteria-rich film coating on the teeth. As that plaque hardens, it becomes tartar, which provides harmful species a place to “hide” and continue producing more acid. This continues to weaken the strength of our teeth by eroding our enamel, leading to cavities: holes in our teeth that develop from dental caries, or tooth decay.
While it is commonly accepted that tooth decay is largely preventable, and even reversible in its early stages via changes in diet, hygiene, and lifestyle, the statistics of tooth decay are staggering. Among adults aged 20 and older, about 90% have had at least one cavity, and over 25% of adults between 24 and 60 harbor untreated decay. A person’s unique oral microbiome and levels of acidogenic bacterial species can help inform his or her risk for cavities, and guide what changes may help reverse dysbiosis.
Gum Inflammation, Gingivitis, and Periodontal Disease
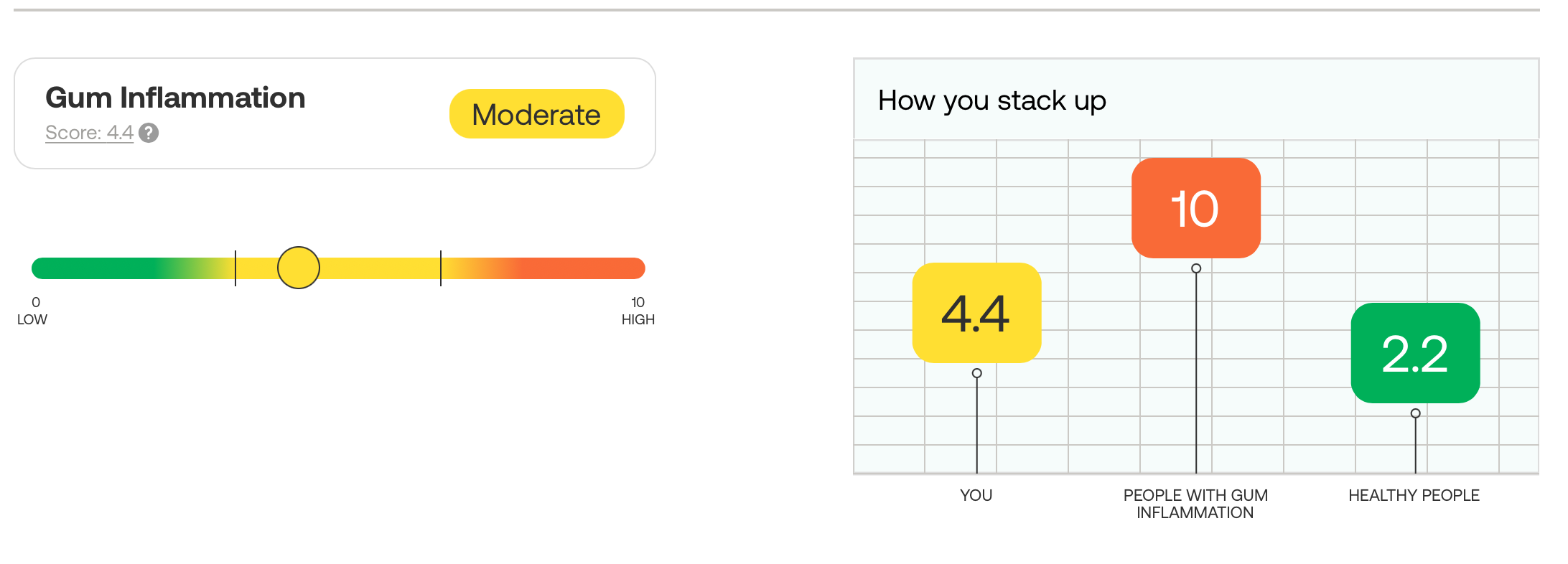
My Bristle results for bacteria related to gum inflammation. Get 15% off Bristle with the code melanieavalon at melanieavalon.com/bristle.
Over half of US adults experience periodontal disease of the gum. Periodontitis is typically broken into 4 stages: (1) gingivitis, (2) slight, (3) moderate, and (4) advanced/severe. Each stage features different symptoms, and the most severe stage may feature bone loss, including the potential to lose some or all of one’s teeth. Periodontal disease is considered to be irreversible past the first stage, and often progresses silently without visible symptoms.
The primary culprit? Specific types of pathogenic oral bacteria.
Gum disease-causing species, such as Porphyromonas gingivalis, are typically anaerobic, meaning they cannot survive in the presence of oxygen. Similar to how plaque turns into tartar, shielding the bacteria that weaken our enamel and causing tooth decay, tartar also acts as a protective shield, allowing pathogenic bacteria to thrive and irritate gums. These bacteria build up around the gum line and release toxins which inflame and damage the surrounding gum tissue, leading to gums which bleed while brushing or flossing. As the disease progresses, these bacteria can cause separation between gums and teeth, allowing for even more plaque to build up. As the pockets deepen, the bacterial buildup weakens the bones and surrounding tissues, instigating bone and tooth loss.
Signs of active gum disease include swelling or redness of gums, bad breath, bleeding or receding gums, and loose teeth. Contributing risk factors include oral hygiene, diet, certain medications, smoking, genetics, hormonal changes, salivary flow/dry mouth, and certain systemic diseases like diabetes.
Halitosis (Bad Breath)
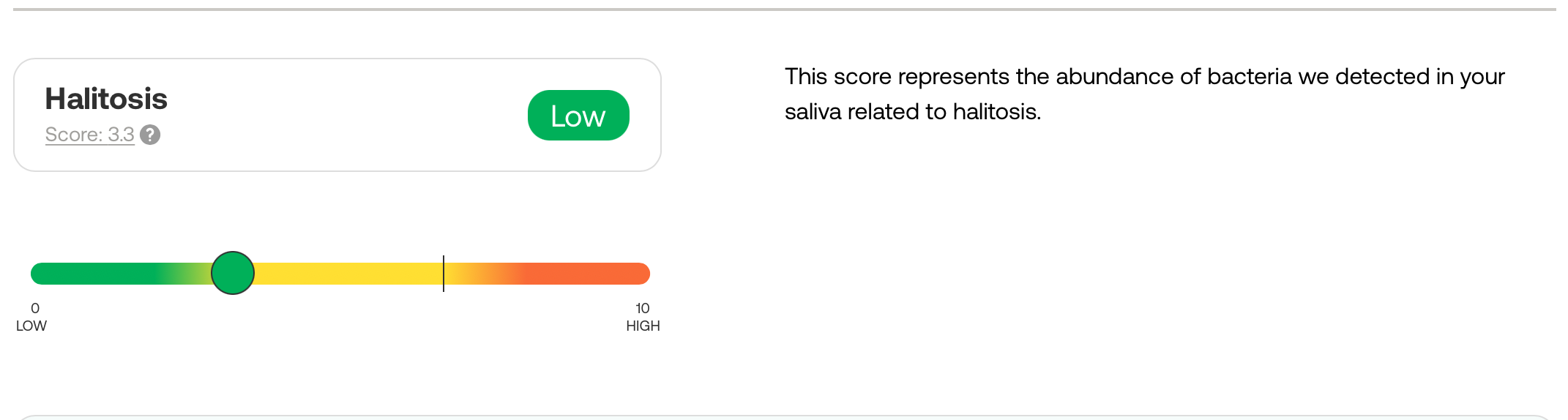
My Bristle results for bacteria related to bad breath! Get 15% off Bristle at melanieavalon.com/bristle with the code melanieavalon.
Halitosis, aka “bad breath” is an incredibly prevalent yet rarely discussed condition, impacting almost 50% of people’s day-to-day lives, causing anxiety and stress in social situations, and, perhaps most importantly, often signaling underlying health issues. Halitosis is not something most dentists treat or even diagnose, leaving patients turning to self research for causes and treatments.
Halitosis causes can be divided into two categories: intraoral (in the mouth) and extraoral (outside of the mouth). Intraoral halitosis is responsible for 90% of halitosis cases, which are caused by a buildup of volatile sulfur compounds (VSCs) that have an unpleasant odor. VSCs include hydrogen sulfide (which creates a rotten egg smell) and methyl mercaptan (which yields a bad cabbage smell).
Oral bacteria are the primary producers of VSCs, with certain species such as S. moorei, P. gingivalis, and P. nigrescens, breaking down proteins in our diet and releasing VSCs as a byproduct. There is a direct association between the abundance levels of these oral bacterial species and the amount of VSCs they produce. The bacteria associated with gum disease are also associated with the production of VSCs, and these halitosis-causing species are often found on the tongue, particularly towards the back, near the throat. Tonsils can also house these bacteria. Wherever they may reside, the bacteria form colonies and multiply, creating biofilm coatings to protect themselves.
Saliva is actually a natural defense against halitosis, containing proteins like lysozymes which attack bacterial cell walls and antibodies, preventing bacteria from settling on our tongue or teeth. As such, dry mouth (low salivary flow rate) is a major contributor to halitosis.
Extraoral halitosis which originates outside the mouth, can be caused by ear, nose, throat, or respiratory diseases (such sinusitis or tonsillitis), chronic diseases like gastric reflux, diabetes, and carcinoma, and medications. Our diets can also contribute to temporary halitosis, with foods such as garlic and onions containing high levels of VSCs.
Mouth-Body Connection
The effects of our oral bacteria and poor oral health extend beyond the mouth, and is associated with a range of systemic diseases and conditions, including Alzheimer’s, cardiovascular disease, diabetes, adverse pregnancy outcomes, and colorectal cancer. In the connected, symbiotic system of our body, bacteria found in our mouths can travel throughout the rest of our body, causing inflammation and a deluge of potentially detrimental downstream effects. We can’t truly be healthy without a healthy mouth.
For a fantastic, comprehensive summary of how oral bacteria impact the rest of our body, check out this comprehensive review by Bristle. For a deeper dive on specific issues, check out these articles on how oral health and bacteria are tied to heart disease, cognitive decline, diabetes, pregnancy outcomes, cancer, and gut disorders.
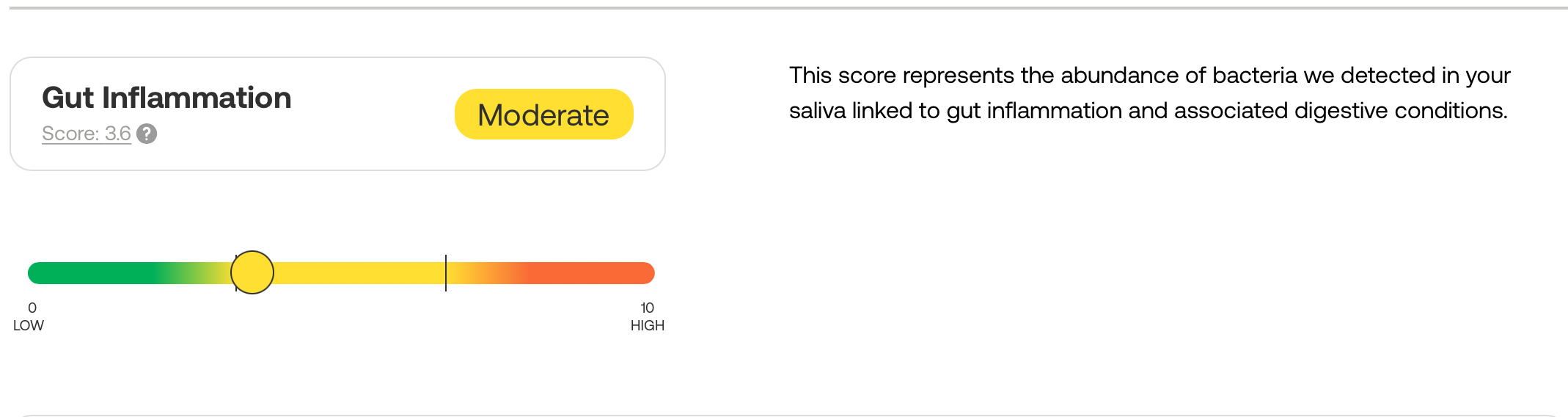
My oral bacteria related to my gut health! Get 15% off Bristle at melanieavalon.com/bristle with the code melanieavalon.
Leveling Up Your Oral & Overall Health
Given the utmost important of our mouth-body connection, how do we avoid dysbiosis of our oral microbiome and get on the fast track to a healthier mouth and body? Here are some tips:
Proper Oral Hygiene
- Brush your teeth twice a day for two minutes to disrupt biofilm formation. While conventional wisdom says to brush right after a meal, food and drink can actually put your mouth into an acidic state. Brushing them during this time risks damaging the enamel, so wait at least 30 minutes after meals.
- Floss with string floss or a water flosser to get into the crevices where bacteria reside, an where your brush can’t reach. (Check out Bristle’s data on how flossing can affect your oral microbiome.) ADD
- Tongue scrape to wipe away the bacterial biofilm on your tongue.
- Beware of certain antimicrobial mouthwashes which can actually cause damage to your oral microbiome by eliminating beneficial bacteria.
Diet & Nutrition
Avoid:
- Sugar and refined carbohydrates: Sugar and candy actually cause cavities because bacteria feed off sugar and release acid as a byproduct, which erodes teeth. If you are eating sugary foods, the key is to eat it all at once: the shorter the span, the less time for feeding.
- Acidic foods and drinks: These include coffee, tea, fruit drinks, soda, sports drinks, sweetened carbonated drinks, and even fruit juices that are naturally high in sugar and acids, including ascorbic acid or Vitamin C. Fruits, especially citrus fruits or dishes like pies, jellies, and jams, as well as candies, fall in the same bucket. If you consume acidic foods, do so over a short period of time, and drink water in between or after, to dilute the acid attacks. Using a straw can help minimize direct contact with your enamel, and always wait at least 30 minutes to brush your teeth.
- Sulfur-containing foods (If you have high periodontal pathogens or existing gum disease): Sulfur-reducing bacteria are key pathogens in periodontal disease, while sulfate-reduction may promote their pathogenesis. Sulfur-containing foods also promote production of volatile sulfur compounds responsible for halitosis. These foods include arugula, asparagus, cruciferous vegetables, animal proteins, dairy, and legumes.
Embrace:
- High-fiber vegetables and fruits: These stimulate saliva production and neutralize acid. They tend to be high in vitamins A and C, which help rebuild enamel and heal gums. These include vegetables like carrots, celery, broccoli, leafy greens, and fruits like apples, bananas, and berries.
- High pH alkalizing vegetables: Certain vegetables have a naturally higher pH, meaning more alkaline and less acidic. These include cruciferous vegetables like broccoli and cabbage, and leafy greens such as kale, arugula, spinach, and lettuce.
- Foods high in nitrate: The oral microbiome plays an important role in nitrate reduction, and nitric oxide production, which is a key molecule responsible for maintaining normal blood pressure. Foods in this category include beet roots and leafy green such as kale, arugula, and spinach.
- Foods with high levels of arginine: Early research shows arginine, an amino acid, can help reduce plaque build-up. Foods in this bucket include poultry, lentils, soybeans, chickpeas, peanuts, and pumpkin seeds.
- Foods rich in vitamin K2: Foods like chicken, pastured eggs, and grass-fed meats can help remineralize teeth and prevent cavities.
- Drinking water and staying hydrated: Water not only helps increase saliva production, but also washes away food particles lingering in the mouth.
Supplements
- Oral probiotics: Some initial efficacy data has shown that oral probiotics like S. salivarius K12 and M18 can help with halitosis and tooth decay.
- Xylitol: Xylitol is a natural sugar alcohol which helps prevent cavities. It reduces the levels of cavity-causing bacteria like S. mutans by disrupting their energy production processes, leading to cell death, less adhesion to teeth surfaces, and reduced acid production. Xylitol also stimulates saliva production, a key component of preventing bad breath. Xylitol is common in many gums and lozenges. (Make sure to check the inactive ingredients.)
The Bristle Experience

Promoting a healthy mouth goes far beyond the simplistic “brush and floss more” mantra, and it all comes down to individuality. In other words, what works for me?
Bristle has made it incredibly easy for all of us to take ownership of our oral microbiome and health. Their at home oral microbiome test measures all 100+ unique bacterial species in your saliva, both beneficial and harmful, to provide an overview of your oral health status. With the data, Bristle then guides you towards an action plan to optimize your oral, and consequently entire, health.
The overwhelming number of products and tips out there are not one size fits all. With Bristle, you can measure your risk for disease over time, and quantifiably see what does and doesn’t work.
Testing Process
You can order a Bristle test (either single kit or subscription) at melanieavalon.com/bristle, where you fill out a short questionnaire. You’ll then receive an at-home kit, in which you collect a saliva sample in a tube. The process takes only a minute or two, and you then send your saliva sample to Bristle’s lab for processing, using an included prepaid return envelope. Results become available via Bristle’s secure online portal, within 2 - 3 weeks.
Results, Recommendations & Coaching
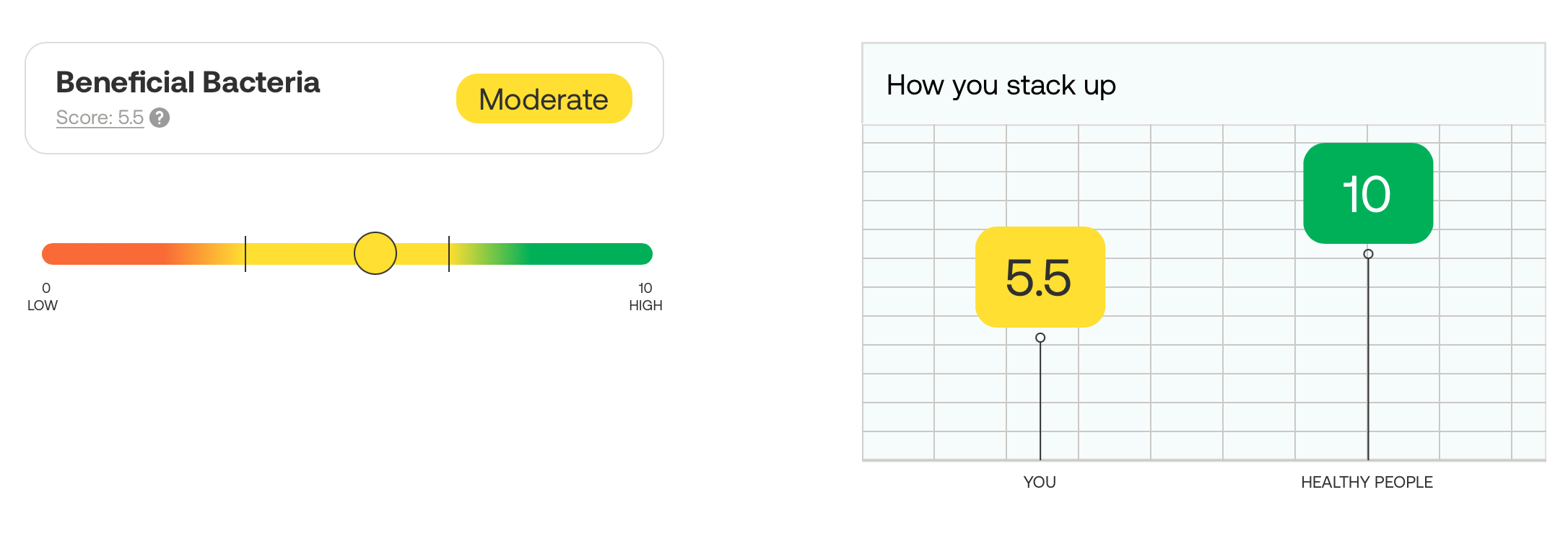
My Bristle results for beneficial bacteria! Get 15% off Bristle at melanieavalon.com/bristle with the code melanieavalon!
Your Bristle report, based on your unique saliva and oral microbiome, features high-level health scores for tooth decay, gum inflammation, halitosis, gut inflammation, and beneficial bacteria. The scores range from 0 – 10, bucketed by “Low,” “Moderate,” and “High” for easy interpretation. You can also see how you stack up against people diagnosed with oral health conditions, such as cavities and gum disease.
Each score includes the contributing bacterial species detected in your saliva, the levels at which they were detected (relative abundance), and a description of the bacteria’s function. You’ll also receive a raw breakdown of all the bacterial species detected in your microbiome, and their relative abundance.
Based on the test results, Bristle provides prevention-focused diet, lifestyle, hygiene, and oral care recommendations that far surpass brushing and flossing. These recommendations focus on oral care product ingredients to look for in products, rather than specific products themselves. Each ingredient recommendation includes a description of what it helps with, how it works, in which oral care products it can be found, and references to research studies.
Of utmost important to me, the recommendations are exquisitely data driven. Bristle also provides a confidence score for the data, based on the amount of scientific research and efficacy data that exists. You can read more about how the Bristle team researches recommendations here.
You also receive access to a 1:1 coaching session with one of Bristle’s oral health and hygiene specialists to review your test results, get any questions you have answered, and work on a tailored action plan together. I did this after receiving my results, with the fabulous Iman (@millenial_rdh), and was blown away by her knowledge, and what I learned!
My Bristle Experience
Testing my oral microbiome with Bristle could not have been an easier, nor more enlightening, process! Collecting the saliva was easy (Who knew thinking of lemons makes you instantly produce so much saliva?), and I received the results in the online portal in a few weeks. It's so cool to see where I stand for beneficial oral bacteria levels, as well the amount of bacteria I harbor related to markers of gum inflammation, bad breath, tooth decay, and even gut health, and how I compare to others!
Bristle provides your raw data as well, so if you're a PubMed junkie like me, you can dive deep down the rabbit hole researching your unique strains! I also love how the recommendations for improvement are non-biased and science based, with notes about the strength of data supporting them, including links to actual studies.
I recently had the pleasure of interviewing Bristle co-founder Danny Grannick, and was blown away by his knowledge and insight! Do not miss my upcoming interview with him on The Melanie Avalon Biohacking Podcast, for the deepest of dives into the science of the oral microbiome!
What’s Next?
I’m thrilled that Bristle provides objective, quantifiable data about oral health. I love that it empowers us as users to measure and track improvement to our scores, and reductions in disease-causing bacteria over time.
The team at Bristle is constantly looking for new associations between the oral microbiome and both oral and systemic diseases, and how different diet, hygiene, and lifestyle factors impact risk for disease. With increasingly more data and research, the delivered insights should only improve and become even more personalized, based on all of our unique microbiomes. Any current or past Bristle users will receive access to future insights as they’re developed.
For anyone who currently faces or has dealt with oral health issues, Bristle helps understand the root causes, and improve with science-backed recommendations. Even if you haven’t struggled with your oral health, testing your oral microbiome can help you take action to improve your whole body health and longevity, given the ties between oral bacteria and systemic diseases. We can’t manage and improve what we don’t measure, and this is especially relevant for our oral health, where trillions of little bugs may be silently wreaking havoc. Thankfully, Bristle shines a flashlight on this oft ignored chasm of potential health knowledge.

