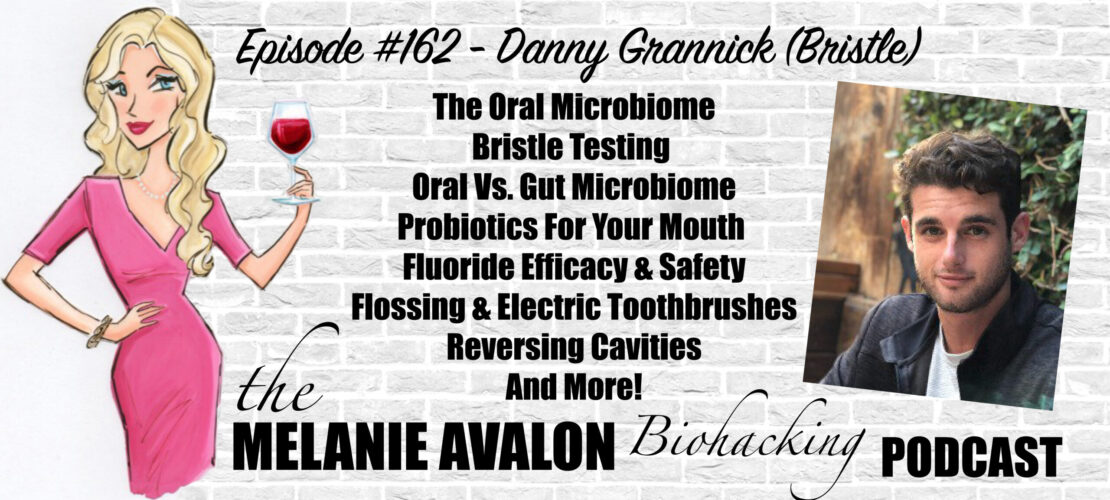
The Melanie Avalon Biohacking Podcast Episode #162 - Danny Grannick (Bristle)
Danny Grannick is the CEO and co-founder of Bristle. He received his BA in Biochemistry from the University of San Diego. After receiving his degree, Danny moved into a variety of commercial roles at Illumina focused on bringing genomic technologies and applications to existing and emerging markets. Danny was then recruited by Oxford Nanopore to lead sales and business development for Northern California in strategic accounts. His passion is in bridging the gap between innovation on the bench and implementation at the bedside.
LEARN MORE AT:
bristlehealth.com
@bristlehealth
SHOWNOTES
Go to melanieavalon.com/bristle and use code melanieavalon for 15% off sitewide!
2:45 - IF Biohackers: Intermittent Fasting + Real Foods + Life: Join Melanie's Facebook Group For A Weekly Episode GIVEAWAY, And To Discuss And Learn About All Things Biohacking! All Conversations Welcome!
3:00 - Follow Melanie On Instagram To See The Latest Moments, Products, And #AllTheThings! @MelanieAvalon
check out my blog on Bristle and the oral microbiome at melanieavalon.com/bristlescience!
3:40 - AvalonX Magnesium 8: Get Melanie’s Broad Spectrum Complex Featuring 8 Forms Of Magnesium, To Support Stress, Muscle Recovery, Cardiovascular Health, GI Motility, Blood Sugar Control, Mood, Sleep, And More! Tested For Purity & Potency. No Toxic Fillers. Glass Bottle.
AvalonX Supplements Are Free Of Toxic Fillers And Common Allergens (Including Wheat, Rice, Gluten, Dairy, Shellfish, Nuts, Soy, Eggs, And Yeast), Tested To Be Free Of Heavy Metals And Mold, And Triple Tested For Purity And Potency. Order At Avalonx.Us, And Get On The Email List To Stay Up To Date With All The Special Offers And News About Melanie's New Supplements At AvalonX.us/emaillist, And Use The Code MelanieAvalon For 10% On Any Order At Avalon X And MD Logic!
Text AVALONX to 877-861-8318 for A 20% off coupon and to keep up with all the latest offers!
7:05 - FOOD SENSE GUIDE: Get Melanie's App To Tackle Your Food Sensitivities! Food Sense Includes A Searchable Catalogue Of 300+ Foods, Revealing Their Gluten, FODMAP, Lectin, Histamine, Amine, Glutamate, Oxalate, Salicylate, Sulfite, And Thiol Status. Food Sense Also Includes Compound Overviews, Reactions To Look For, Lists Of Foods High And Low In Them, The Ability To Create Your Own Personal Lists, And More!
7:45 - BEAUTYCOUNTER: Non-Toxic Beauty Products Tested For Heavy Metals, Which Support Skin Health And Look Amazing! Shop At Beautycounter.Com/MelanieAvalon For Something Magical! For Exclusive Offers And Discounts, And More On The Science Of Skincare, Get On Melanie's Private Beautycounter Email List At MelanieAvalon.Com/CleanBeauty or text BEAUTYCOUNTER To 877-861-8318! Find Your Perfect Beautycounter Products With Melanie's Quiz: Melanieavalon.Com/Beautycounterquiz
Join Melanie's Facebook Group Clean Beauty And Safe Skincare With Melanie Avalon To Discuss And Learn About All The Things Clean Beauty, Beautycounter And Safe Skincare!
13:00 - danny's background
16:50 - danny's personal oral Hygiene habits
18:55 - the history and research in oral health
21:30 - red & orange complex
23:45 - bacteria and its relationship to oral disease
29:00 - what bristle tests for
31:10 - publishing clinical literature
32:30 - the range of results
35:20 - implications of diversity in the biome
Bristle Research: How Oral Microbiome Diversity Impacts Oral Health
37:55 - is there overlap in species in oral and gut microbiomes?
40:00 - how many species are in the gut?
40:20 - what types of organisms inhabit our oral microbiome?
41:00 - what determines our biome make up?
43:05 - how quickly can it change?
48:30 - transient and colonized bacteria
51:10 - what is the method of transit?
52:55 - can you reset the oral microbiome? what happens?
56:55 - fermented foods
57:40 - dental carries
1:03:35 - LMNT: For Fasting Or Low-Carb Diets Electrolytes Are Key For Relieving Hunger, Cramps, Headaches, Tiredness, And Dizziness. With No Sugar, Artificial Ingredients, Coloring, And Only 2 Grams Of Carbs Per Packet, Try LMNT For Complete And Total Hydration. For A Limited Time Go To Drinklmnt.Com/Melanieavalon To Get A Free Sample Pack With Any Purchase!
1:06:40 - do cavities always indicate disease?
1:12:45 - how fast does bacteria begin to effect the teeth?
1:13:40 - should you brush immediately after eating?
1:15:25 - nitrates, nitrites, Nitrosamine
1:17:10 - the bristle program
1:19:10 - the importance of flossing
1:22:05 - electric toothbrushes
1:25:00 - how often should we replace our toothbrushes?
1:27:30 -the bristle results
1:31:30 - is there any downsides to getting fillings?
1:33:00 - the bristle recommendations
1:35:00 - Oura Ring: Monitor Your HRV, Sleep, Stress, Activity Levels, Respiration, Body Temperature, Oxygen, And More! For a Limited time Get $30 Off At Ouraring.com/melanieavalon!
1:37:15 - Fluoride efficacy and safety
1:43:15 - one on one consultations with bristle experts
1:45:00 - what is the future of bristle?
1:48:00 - hSA and FSA Eligibility
Go To melanieavalon.com/bristle And Use Code MELANIEAVALON For 15% Off Sitewide!
TRANSCRIPT
Melanie Avalon: Hi, friends, welcome back to the show. I am so incredibly excited about the conversation that I'm about to have. Okay, the backstory on this conversation, there is a topic that we talk about a lot on this show, and that is the microbiome. That said, I think when people hear microbiome, they think the gut microbiome and historically, that's what all the episodes on this show concerning the microbiome have been about. That said, I have been very intrigued at the implications of the oral microbiome. Maybe we can touch on this later in the episode, especially-- well, I had been just in general, thinking there probably is something there, especially since it took us so long to finally understand the implications of the gut microbiome. And then on top of that, I remember I read a study a few months ago talking about how maybe some of the GI issues that we thought were due to gut microbiome imbalances, particularly SIBO being caused by the microbiome from the colon migrating up, that actually, it might be due to the oral microbiome migrating down, which blew my mind. And when I heard that, I was like, there's a lot going on in the oral microbiome, and nobody's talking about it.
So, I've been wanting to do an episode on it. And as the way things often happen, the perfect person to do this interview just came to me. There's a newish company called Bristle. Friends, this is the coolest thing ever. They provide a super easy, at-home oral microbiome test, super easy, just requires some saliva, you send it off. And then, you get personalized results that show information about your oral microbiome, as well as recommendations and a care plan. And they're even setting up a system where you can do a one-on-one call to learn about your results. And I did that and was blown away by the information.
On top of that, and I was just telling the cofounder before we started recording, their log that they have associated with their website is next level. I know you guys often like my blog, for example, because of how it goes into the science and the detail and has studies. This is like that times 10. They have posts about all of these topics, and it is so incredibly nuanced and so enlightening. This whole process has just been absolutely amazing. I've been looking forward to this for so long. I am here with the CEO and cofounder, Danny Grannick, I have so many questions. Danny, thank you so much for being here.
Danny Grannick: No, thank you for having me. I'm super excited. Let's do it.
Melanie Avalon: And on top of that, Danny gets all of the awards because I put him through the wringer before recording with getting a better mic, and he literally drove to have a better setup. So, I thank you so much, Danny, for your patience and your time.
Danny Grannick: All of the awards or none of the awards, because I also didn't have the microphone for the session at the beginning. I'll take that one.
Melanie Avalon: Well, here we are now. I'm just so excited about this. Like I said, so many questions. But to start things off, I am so curious about you. What led you to cofound this company? Because that is no small feat, cofounding a company, especially one that is so incredibly interactive. You're not just creating a product. You're creating an interactive experience and education. And I mean, there's a lot that goes into this. So, what led to that? Also, were you always interested in the oral microbiome or when did that interest start? What is your story?
Danny Grannick: Yeah, I get asked that a lot. I think even my friends are still kind of surprised when I'm talking about the company to hear that it's in oral health. I never imagined that I would end up here. My background is in biochemistry. And then coming out of college, I was making the decision that a lot of people have, which is, do I go pursue my PhD in something very specific in science? Or do I kind of branch off and do something else? That something ended up being a career in genomics on the commercial side, actually, and I worked for a sequencing company called Illumina. They make the platform technology that other companies use to do genetic sequencing. And it was a really exciting time to join.
Genomics have largely been more on the research side. When I came on, there was this transition into the clinical side. So, sequencing was being adopted into companies into your care systems. It was being applied across oncology, noninvasive prenatal testing. We are seeing this really exciting set of improved health outcomes on the other side, shifting to this more precision based and preventive standard of care. So, I was blown away. It was awesome to see the application of advanced technology touching all of these different areas of health. I had always been entrepreneurial, kind of looking for the next opportunity where I could make an impact. And that was kind of where it stopped for a while. I think I was so swept up in the innovation in the industry that I wasn't really focused on starting anything.
And it wasn't until a couple of years in when I was living in San Francisco that my now cofounder, Brian, and I were just watching a pitch competition at UCSF, so University of California, San Francisco. There were a couple companies that were presenting on the gut microbiome, which we all know has exploded over the last couple of years. And we were sitting in the crowd. We had worked with almost every company in that space. And Brian, by chance, had a dental appointment the next day. Probably like a lot of people listening right now, Brian is this like cliché patient who is religious about oral hygiene and always would get cavities. Every time he would go to the dentist, they would find a cavity. He'd be back in a couple of weeks for fillings. So, he was lamenting about this impending dental appointment. I think it was just this really serendipitous context of listening to the pitches and talking about Ryan's dental appointment that we started really asking ourselves, why we hadn't seen any companies in the space, tackling oral health with something other than x-rays and observational screenings? And that led us on a journey of research and interviews and cold emails to researchers at universities for about a year and a half, just trying to understand how the oral microbiome was connected to oral health and then doing a really deep dive into the standard of care and how we think about oral health and whether or not leveraging the oral microbiome could bring the improvements to the standard of care that we wanted to see.
Melanie Avalon: Wow, I feel like I could have a whole episode just on the entrepreneurial side of this because I am so fascinated by it. For the journey for you through this whole experience, have you changed your oral habits?
Danny Grannick: 100%. I am probably another cliché and probably like a lot of other people that are listening to the call. When I was five or six, I was diagnosed, I think it was six or seven cavities at the same time and they all needed fillings. You can imagine that kind of appointment and that kind of procedure for a five- or six-year-old was a pretty traumatizing experience. So, I have hated going to the dentist ever since. To me, the experience makes my skin crawl. The smells, the sound of the drill, the fear that I'm going to go and find out the same stuff that Brian always does, which is I have a cavity and I need a filling. I was diligent about my oral hygiene. I think unlike Brian, I fell into this luckier group, which was, I did the basics, and I was lucky to never have oral disease since that event.
But for me, it was, yeah, it was kind of the opposite story. I think my oral hygiene was just the bare basics. I was fortunate because I never had tooth aches or pains or anything to really drive me to the dentist beyond the typical checkups. Since starting Bristle, I think that there's this change in perspective. As we were researching the company and uncovering the connections between the oral microbiome in oral health and oral and overall health, it all of a sudden became apparent that this aspect of my health that I had overlooked for so many years and kind of written off as just a set of chores that I had to do is actually a really important component of maintaining and improving my health. Since then, obviously using Bristle, I've been able to implement new steps in my hygiene routine, I've switched the products that I'm using, and I've been able to track the impact of that on my oral microbiome ever since.
Melanie Avalon: I do have a really granular question about the cavities. But before that, I guess just stepping back, when you started going through that process that you spoke about with gathering research and cold calling and learning about this, in the scientific literature, how many studies are there? What did you find when you sat down to research?
Danny Grannick: Yeah, the history of research around it. I tend to separate it almost into two categories of research around oral health and research around the oral microbiome. Obviously, there's overlap, but it's a really interesting history. We can actually go back to, I want to say, the mid-1600s. And there is this guy, and I'm going to totally butcher this but it's Antonie van Leeuwenhoek. He was an early scientist, he's deemed the father of microbiology, and he had changed his career to focus on creating lenses and eventually, obviously, started creating the early versions of what we know as a microscope. And he would basically go around, and he was starting to look at different objects under these lenses.
He wrote a foundational paper, where he described some of the earliest, if not the first, descriptions of microbes, and it was called concerning-- it's translated, but it's called Concerning Little Animals. He called them "animalcules". You can imagine this guy is going around his house or his apartment, or whatever, and he's looking at all of these different things and seeing all of these different organisms and moving around. I believe the first biological sample that he looked at was actually a sample of dental plaque from his mouth. When you look at those early pictures, there is a drawing of the microbes that he saw, having taken dental plaque off of his teeth, and put it under the microscope. When we think about microbiology, I think a lot of people probably defer to environmental microbiology, and obviously, gut microbiology, and all of that kind of stuff. But it really is rooted in the oral microbiome, which is kind of an interesting little tidbit.
But obviously, going off of that, over the next couple centuries, we continue to do research into the oral microbiome and some of the earliest expansions on our understanding concerned very specific bacteria and their association to gum disease. There is something that's taught in a lot of dental schools, it's called the red and orange complex, and it's 12 or 13 species of bacteria that had been identified in very early research as being causally related to the onset and progression of gum disease. Most of the research since that kind of criteria, that category was established has really been limited to those bacteria. When we look at a lot of the research in oral health and oral microbiome, it's contextualized to those 12 or 13 bacteria, and that was it for a really long time. The same thing was done with carriers where cavities causing bacteria, there were five, maybe six that we'd identified. And all of the research just looked at those bacteria in the context of health and disease. So, it was a very narrow understanding. And for context, since then, we've identified over 700 bacterial species as being part of the oral microbiome. And a lot of that work was done by a research group out of Harvard called the Forsyth Institute, and in the NIH, who created the human oral microbiome database. They were able to expand the catalog and our understanding of the oral microbiome and its role in oral health.
Since then, it's still just remained in this very narrow scope. A lot of the research papers that have been released have not gone past that red and orange complex. They've only looked at one or two species of bacteria. But I think the exciting thing is that our understanding between oral health as a category and overall health has progressed a lot. There's been a history of associations between poor or declining oral health and systemic conditions, some of the major ones, including cardiovascular disease, Alzheimer's, diabetes. And for a long time, it was really only shown at the clinical or symptomatic level where we could correlate somebody with declining oral health would also have some kind of systemic disease associated with it. But we're now able to look at that in this very empirical and objective lens by looking at the comprehensive oral microbiome, and we're starting to uncover more concrete connections between those indications.
Melanie Avalon: I just want to say how much I'm enjoying this conversation. Okay, some questions about that. This is something I was thinking about when I was reviewing a lot of the literature on the Bristle blog and also looking at my results, and it would say that-- we're talking about how these different strains, you have shown connections to different oral mouth issues and you just spoke about, like they would study, related to dental caries, or gum disease or whatever it may be. When they say that a certain strain has been found to be beneficial for bad breath or gum inflammation or something like that, out of those 12 or so main strains, have they done tests on all of them for all of the conditions? Or is it more like some of them, they've tested for some things and some for others? The reason I'm asking is it can make it seem like, "Oh, this is the strain that's good for bad breath," but is it just because that's the strain they tested for bad breath, and they don't actually test all the other strains for bad breath? Does that make sense?
Danny Grannick: Yeah, you're hitting on a really good-- So, there's two pieces there. When we think about the progression and research, there's breadth. So, the idea of expanding to your point, when we have done research in the past and tested for bacteria, we've really only tested for those 12 or 13 and you don't know what you don't know. So, if you're only testing for 12, or 13, but there's 100 different species of bacteria in somebody's mouth, you're missing the complete picture. You're making assumptions based on what your test is saying is there, isn't there. And you're also limiting your understanding of what bacteria causes diseases to what you're testing for. It's a very narrow, kind of shielded horse blinders way of looking at biology.
And then we have the other concept or the other piece, which is depth. For a long time, including the red and orange complex, we'd only looked at microbes at the species level. But advances in sequencing technology allow us to look at the strain level. So, multiple strains of bacteria can make up a single species and not related to oral health, but I think a really good example is E. Coli. Everybody is really familiar with E. coli as a species of bacteria. But the reality is that there's, I think, dozens, more than 10 different kinds of strains of E. coli, and only a few of those strains are pathogenic, the ones that kind of migrate their way into-- I won't mention specific companies, but food that you would get from a restaurant that leads to some pretty unwanted side effects.
But it's important to understand what strains are present. And that requires higher resolution technologies, because you would want to know as a consumer, if you're about to eat a salad, and you're only testing for the species of E. coli, it may come up positive, but the strains of E. coli that are in that salad may not be the ones that lead to those symptoms that nobody wants to deal with. They may be unharmful or even commensal species, so beneficial species. And that's been a really big turning point in the oral and gut microbiome and our understanding of the role of those microbes in health, because we're able to deconvolute the presence of not only a species of bacteria, but specific strains and the role that they play. It's kind of two levels of resolution that we've been able to develop. And then, we've also been able to just test for more species at the same time. So now, we can look at all of the microbes in a given sample instead of only limiting research to detecting whether or not those 12 or 13 predetermined targets are there or not.
Melanie Avalon: With those 12 or 13 initial ones, did you find that the majority of them were tested for all of the different conditions or was it lacking in that area?
Danny Grannick: I think the 12 or 13 in the red and orange complex associated with periodontal disease are very much associated with periodontal disease. I don't know if outside of Bristle, they've been compared against other conditions. I do know that systemically they have been so-- to name another example, P. gingivalis a notorious oral pathogen, it's in the red complex of the really, really bad section of that pyramid of bacteria. That species of bacteria is causally related to the onset of periodontal disease. And there have also been research studies looking at that species of bacteria in the context of Alzheimer's manifestation and progression. We have found that certain species of bacteria do overlap and indications. We see, for example, that a lot of the species that cause periodontal disease are also implicated in halitosis or chronic bad breath. But again, when you're only looking at 12 or 13 species for all of your research, you're missing the role of the other 80, 90, or 100 species that are present in somebody's mouth. So, you may be making assumptions or seeing correlations that aren't actually true, signals that may appear stronger than they actually are and vice versa. So, we're finding new species that are associated with periodontal disease and with caries and with halitosis. And we're also able to develop new insights about new bacteria that may be associated with overall health and disease including gut dysbiosis.
Melanie Avalon: So, with Bristle, do you test over 700 strains or species? Strains?
Danny Grannick: Yeah, that's a good question. We use a method called shotgun metagenomics, and the name isn't important. The idea is-- let's actually back up. A lot of people are now familiar with qPCR because of COVID, obviously. And the way that qPCR works is you predetermine targets, genomic targets of, in this case bacteria that you want to test for. So, I could say, "Okay, I want to test this sample for these 10s species of bacteria." And what that test will tell me is whether or not they're there. And if they are there, what their relative abundance is within that sample. But there could be 150 species that are actually in the sample, but I won't know because I'm only testing for those 10. And that is going back to that red and orange complex, and a lot of the research that's been done to date.
Our technology sequences everything in the saliva. We don't predetermine targets. We don't make assumptions about what's there or not. We sequence everything and we get the whole genome information. And then, we map it to this massive database of potential species. And in some cases, we're actually assembling new species ourselves and doing discovery in that sense. Yeah, and that allows us to pick up on anything that's on there.
Melanie Avalon: I feel like that's a big deal [laughs] Like, that's a really big deal.
Danny Grannick: Yeah, it's really important. I think the other microbiome industries and other tests that are on the market, they can be really effective in confirming the presence or absence of species that we already know. But a big part of Bristle is progressing our understanding of the oral microbiome. So, we wanted to invest in a technology that would produce as much data as possible whether or not we know that those species of bacteria at this moment in time are associated with health and disease, we want to be the ones to make those associations and make those discoveries and then present them to our users.
Melanie Avalon: Are you guys publishing clinical literature on your findings?
Danny Grannick: We have had an ongoing clinical research collaboration with the University of the Pacific and San Francisco, the dental school there. They were actually some of the earliest supporters of Bristle before it was ever a company when Brian and I were just emailing random researchers. So, I do want to give them a very sincere thank you and a shoutout on the podcast. We've been doing a clinical research study, and that was how we kicked off the company. And that study takes patients that go to the dental clinic, and we obtain a saliva sample before their checkup. And then, we get the full record of that dental checkup as well as their electronic medical record. So, we can look back and start to tease out associations between the oral microbiome status of a given patient cohorts, and not only the dental symptoms that they had that day, but also other aspects of their health including overall health as well as previous oral health conditions.
Melanie Avalon: Wow, that is super, super cool. If you are testing for literally everything-- because when people get the results, they get like a summary and then with a lot of really helpful information kind of grouping the bacteria into how it relates to different conditions that people might experience. But then, you also get your raw results. I pulled up my raw results, which actually list the genus and the species and their relative abundance. For that list, because I looked at mine, and there's around like 60 species listed, does that mean there potentially could have been up to like 700? And what is the range that you see with people? Some people have like one?
Danny Grannick: Yeah, so that list-- I guess, going to the report, having looked at the genomics industry and worked with the companies for a while, one thing that we wanted to bring to the product was just when people take the test, it's generally I have a problem, and I want to understand what's causing it and start improving. We wanted to make that understanding as easy as possible. So, we want to boil down the complex data into very readable, easy-to-understand scores. But there is this really exciting research and discovery aspect. And I think that a lot of our users want to leverage the data to do their own digging and start to read up on various research papers and new discoveries, because obviously, we're a small team, and we can't even keep up with everything ourselves. So, we've had different users email us new research studies, and that's always nice to get.
But with regard to the raw results, there are over 700 species associated with the oral microbiome. That generally means that-- and again, that is always expanding. But that generally means that as a person, you will have some combination of any of those 700 species. It doesn't mean that you have all of them. On average, we usually find somewhere between, I would say, 60, 75, to 120 different species in somebody's oral microbiome but there are certainly exceptions to that standard. We have users that take the test, and they only have a handful of microbes. And that's really been an exciting piece of research internally, because having that low of a diversity in your oral microbiome, in some cases, hasn't manifested in any sentence and it's been a surprise to the person who took the test and other cases, it has come from a user who has had chronic oral disease for a really long time, they've gone through the gambit of interventions, and nothing has worked. So, we do have these outliers that that take the test, and for us, it's an opportunity to start to understand at a community level of how the oral microbiome connects to health and disease, and also start to work on more effective interventions and care paths for these patients to repopulate and restructure the oral microbiome into a healthy state.
Melanie Avalon: Okay, that is so fascinating, because it's really analogous to the gut microbiome in a way. Because I feel like with the gut microbiome now, the thing everybody talks about is diversity and how that correlate to all of these beneficial health effects. But then, or and I've seen a lot of studies on the gut microbiome in patients with low diversity who actually experience less symptoms. And it's kind of like you said, like this outlier situation, although I might have made an assumption. In general, is more diversity in the oral microbiome correlated to better health in general? Oral health?
Danny Grannick: Yeah, that's one example of a piece of research that hasn't really been looked at, because the technologies that have been used for the most part have been those kinds of narrow pieces. You can't understand diversity in an environment if you're only looking at five species of bacteria, and that's it. So, we've been able to build a new understanding of the role that diversity plays in oral health. It's ongoing. I think early signs kind of tell us like you would expect, that it's a bit of a bell curve, where you want to land somewhere in the middle. And too high of an oral microbiome diversity is potentially associated with adverse outcomes. Same thing with low diversity. We actually have a blog article that we published with some internal research and data for what we've seen with regard to diversity. I would highly recommend anybody listening, go check it out.
Melanie Avalon: Oh, I will put a link to that in the show notes. And by the way, the show notes will be at melanieavalon.com/oralmicrobiome, I just want to clarify. So, you have seen with some of your results that people with high diversity actually correlates to issues? That's really interesting.
Danny Grannick: Yeah, it's kind of the combination. I don't think it's ever going to just be diversity that affects somebody's oral health or overall health status. We have to look at the identity of the microbes that make up that environment. Having an ultra-high diversity of all commensal species of bacteria is probably great but having an ultra-high diversity in a lot of pathogenic species obviously wouldn't be-- And part of it is understanding what the balance is between those two. So, somebody may have a very high diversity and if they have more commensal species or strains as part of their oral microbiome, it may actually help mitigate the risk that the pathogenic strains in their oral microbiome convey. So, they could have relatively high abundances and a few different varieties of pathogenic bacteria, but there is kind of this community level effect where the negative effects of those pathogenic bacteria are-- I don't want to say cancel the help but combated.
Melanie Avalon: Is there overlap between the gut microbiome and the oral microbiome with any of the strains? Or do they tend to be two completely separate communities? I mentioned at the beginning, I'd read that study about SIBO potentially being related to oral microbiome migrating downwards. Yeah, what is the comparison there?
Danny Grannick: Yeah, I think it always comes back to-- for a long time, and we still continue to think like this sometimes, but we have traditionally looked at the body as this very compartmentalized modular organism where our mental health is its own thing and our cardiovascular health is its own kind of self-contained box, metabolic health. And that's not how our bodies work. It's an ecosystem and everything influences something else. So, the gut and the oral microbiomes are obviously physically connected by our digestive tract. But for a long time, there weren't known associations between those two. What has been uncovered over the last couple of years, I think through research has been that certain oral bacteria can migrate to the gut and cause dysbiosis or adverse effects there.
There are even cases where commensal species of bacteria, so species in our oral microbiome that are beneficial to our oral health can migrate to our gut, and when you change the environment, they become pathogenic to that environment, so they can actually end up causing damage. Specific strains have been-- I'm going to say P. gingivalis a lot because it is kind of the most notorious and one of the most well studied, but F. nucleatum, as well has been tied to gut dysbiosis, IBS, IBD, Crohn's disease, colorectal cancer as well. And I think that we'll continue to uncover the relationship between oral health and gut health and vice versa. We also see that gut dysbiosis can manifest as oral disease in the same way that we've seen with diabetes and some other chronic diseases.
Melanie Avalon: Do you know how many in general-- this is something I should know, how many species in the gut, they now think that there are?
Danny Grannick: Oh, I don't know off the top of my head.
Melanie Avalon: I'll look it up and put it in the show notes. I should probably know that. Another question looking at the gut some more. There's bacteria, but then there's also yeast and parasites-- and I always say it wrong, archaea? Is the mouth pretty much just bacteria or are there other organisms as well?
Danny Grannick: There's the full breadth of organisms that you find in other environments, viruses, fungi, bacteria are typically the main three. That's another advantage of our test. Because we use shotgun metagenomics, we actually detect and can identify all kinds of microbes, I think different from the gut, our understanding of the role of those other microbes in oral health and overall health is so early. So, we're doing a lot of research there. But we do plan to release that kind of data as part of the raw results so that people can start digging in on their own.
Melanie Avalon: Okay, awesome. Do you know or have there been studies on what determines a person's oral microbiome? Are we born with it? Is it affected by birth? Is it inherited? What creates it?
Danny Grannick: Yeah, so the research is still early but there's a couple of factors. The biggest one is behavior and environment. The emergence of pathogenic bacteria, the prevalence of oral disease is largely a byproduct of poor oral hygiene, poor dietary choices, things like that. But there have been some studies that have shown-- when we're born, there have been studies that show more similarities in a children's oral microbiome with their mothers. There have been studies that have shown actually that the oral microbiome and the placental microbiome are more similar than-- I think it was the oral microbiome and the gut microbiome or the placental microbiome and the gut microbiome, one of those two. So, there is this idea that parents can confer oral microbiome signatures to their children. And then, that in combination, I think with behavior and hygiene habits, which are also conferred from parents to children. So, any parents out there and make sure you're brushing your teeth in front of your kid all the time.
I think it's similar to our genetics. You get some blueprints from your parents but a lot of what happens later in life and a lot of the things that you may be at risk for materialize based on other factors that influence the expression of those genes. And the oral microbiome is similar. We also find that oral microbiomes can be influenced by our partners. So, a lot of spit being exchanged between romantic individuals. For the record, cavities have been, I think, labeled noncommunicable, but I would argue with that. I think that it is a communicable condition. So, we do see some similarities in in couples that that live together and again, parents and children.
Melanie Avalon: And how fast do changes tend to happen? One of the blog posts that you had was fascinating. I think it might have been--was it effects of flossing, or-- okay, one of your blog posts was talking about the oral microbiome, and it was talking about having different strains and what they affected. And it was saying in some of the studies, that maybe in order for these oral probiotics to be taken and have an effect, that you had to first wipe out your microbiome with an antiseptic for it to have a full effect, which was a really fascinating concept to me. How fast do changes happen in the oral microbiome in the mouth? If you use an antiseptic, do you just wipe out everything? What's happening there?
Danny Grannick: Yeah, there's a lot to unpack. I think the blog article was on oral probiotics. I would highly recommend people read it. We have a lot of information about probiotics, and I think that there's also a lot of misinformation out there that we touch on. But we are finding that there are dependencies on how quickly you may be susceptible or can recover from oral microbiome dysbiosis or oral health conditions based on the oral microbiome profile that you have. We're starting to understand loosely these buckets of oral microbiome profiles and that can help us predict somebody's risk for progressing to oral disease as well as stratifying the efficacy have different interventions. Like everything else, the rate of progression depends on the environment, your behavior, as well as your specific oral microbiome. But we know that people go from healthy to disease between dental visits, like Brian. So, it is a pretty rapid progression from a healthy state to a dysbiotic one in the majority of people.
As far as the use of probiotics, so probiotics, it's not a great comparison but I always talk about vitamins as kind of an analogy to probiotics. If you meet your daily intake of vitamin C every day, taking a vitamin C supplement that's at 2000%, you're not retaining 2100% of your daily intake of vitamin C and becoming like a superhero. Your body's flushing out a lot of the excess vitamin C and our microbiomes, and the use of probiotics works similarly. So, the efficacy and the potential that you're a good candidate for a probiotic does depend on the oral microbiome that you have. One probiotic is called K12, and it's an S. salivarius strain. It's a beneficial strain of bacteria that's in the oral microbiome or was found in the oral microbiome of healthy individuals. There's a bunch of research on it being effective. But if you already have a high abundance of that species or strain and your oral microbiome, introducing more of it is not going to-- or reduces the chances of a significant shift in your oral microbiome makeup, and therefore your oral health status. So, we're finding that the best candidates for certain probiotics are the ones that have the lowest abundance of that species to begin with and then we kind of reintroduce that species to increase its abundance.
The other really cool thing about the mouth, I think, talking about antiseptics, one way to, I guess, artificially decrease the abundance of either beneficial microbes that you want to reintroduce or pathogenic bacteria that you want to further eliminate is just by kind of wiping the slate clean. And traditionally, that has been done with antibiotics, antiseptics. They're definitely effective in wiping everything out. Our ability to rebuild the microbiomes in a predictable and intentional way, I think, is still some ways off. Which is why you see a lot of patients, I think, especially on the gut microbiome side that have kind of bombarded their gut microbiome with antibiotics, and then have resulted in more severe symptoms and they had to start, and now they're at a dead end. And they're going through the full wringer of trying different probiotics and different medications.
The cool thing about the mouth, something that makes me really excited about the potential is it's one of the only parts of our bodies that we can physically manipulate. Outside of our skin that you can rub soap on or put something on or scrub, our mouths are the only other place that you can mechanically use a toothbrush, or a tongue scraper, or floss to physically remove bacteria from the environment. And that in combination with more controlled use of antiseptics and antibiotics, I think, is the best and most effective path to wiping the slate clean and giving yourself the best chance to have a high response to the reintroduction of probiotics. And those are the kinds of care paths that we're developing for our users.
Melanie Avalon: In the gut, they often talk about how there's basically-- and maybe there's some overlap, but basically two broad types of probiotics in the microbiome. The ones that that are there that are like colonized. And then the ones that are transient, when we take probiotics and they kind of pass through when you stop taking the probiotic, they go away. In the mouth, are they all transient? Or are there some that are kind of like similar to the gut microbiome where they're there? And they stay there?
Danny Grannick: Yeah, we're still looking into the transient aspect. But I think a lot of the research and the provided to us today points to the end goal being to recall an eye a microbiome environment by eliminating the pathogenic species of bacteria and replacing them with probiotic or beneficial species. And that's what we're trying to do with the oral microbiome first. Like you said, I think there may be some efficacy and transient probiotics, but that also ends up-- I think it's a band aid, and it also causes a dependency on taking them all the time and we also don't completely understand why they're not they're working.
I think that one of the problems with probiotics is unless you're really diligent about testing, there's no way to actually know whether or not you're shifting your insert whatever microbiome you want into the state or the makeup that you're trying to go for. And there's a lot of companies on the market that are just selling probiotics, and all of these probiotics have the same strains or some combination of the same strains. And there's no way to one-- I mean, there are ways. There's got microbiome tests on the market, but I think only a fraction of people really use them. But it's important to understand where you're starting from and also map and kind of track where you're trying to end up because you can take probiotics for six months but if you test between-- if you do a before and after test, and you don't see a shift in your microbiome, you might be feeling better, but because you're taking the probiotics, it might be a placebo effect. It might be some other kind of intervention that's been introduced. So, I think the probiotics are available, but in terms of really being able to quantify their efficacy and, and landing and expanding in the microbiome that you're targeting. There's still a ton of research that has to be done.
Melanie Avalon: And major question about this. And I have wondered about this for so long, and it's really important for the conversation we're having right now. The method of-- if you are taking those probiotics, because they're often sold as a pill, like a capsule, if you're doing that, do you take it, it goes down to your GI tract, and then they may work their way back up to your mouth? And/or how does that compare to a lozenge, because I was looking at some of the studies and they would use lozenges, and or like a probiotic toothpaste? So, the actual method of how they get to the mouth?
Danny Grannick: The method definitely matters. I don't think that there's been enough research in swallowing probiotics and showing a true shift in the oral microbiome profile. We have seen stronger studies with lozenges. I think there's maybe a few toothpastes on the market. Mouth rinses something else that I'm really keen on looking at. Obviously, not with alcohol, and antiseptics, and all that stuff. But there's a lot more ways to introduce probiotics to the oral microbiome and/or with the gut microbiome and that provides almost this targeted methodology, I think it would be really cool to see one day like a floss and that floss is coated in a very specific probiotic bacteria, and you're introducing it exactly where it needs to go. Same thing with mouth rinse and your tongue or tongue scraper. And then, you can imagine a toothpaste with kinds of probiotic bacteria that mitigate the growth of S. mutans, one of the key players in cavities formation. There's all of this potential, because you can literally open up your mouth and access it.
Melanie Avalon: Oh, my goodness. If you ever want to collaborate on something in the future, I would so be down. That's amazing. I would so be down for this. Okay, some other questions while we're still talking about the oral probiotics. One of the most fascinating findings, sort of recentish, on the gut microbiome was a study where they were looking at wiping out the gut microbiome. I think it was a colonoscopy prep. So, it wasn't antibiotic wiping out, but it was wiping out, I guess, physically. And they found that the person's gut microbiome returned to their "normal" microbiome better if they didn't take probiotics. So it was like a natural process, to just let it happen. In the mouth, do you think there's a difference in, say, "wipe the slate clean" like we keep talking about, like, the effects of that, will it kind of go back to what it was before compared to if you do integrate some sort of probiotic, are you changing what it becomes? I know you touched on this a lot already but I'm just curious if the mouth kind of naturally gravitates to the state it was at before and how factors might affect that.
Danny Grannick: Yeah. Full disclosure, I would love to see the study. So, this is all conjecture for the record. My guess is that-- okay, so we have used the term 'wiping the slate clean', and I think that can mean different things to different people. Just like if you're living with roommates, my standard of clean might be different than my roommate standard of clean where when I wipe down a counter, it's bleached, and I'm putting elbow grease into it and I'm spending an hour. Whereas somebody else's definition of wiping the slate clean or cleaning your counter might be taking a dirty rag with some water on it and just kind of wiping it down a little bit. So, with that gut microbiome study, I'm interested to look at it because my first response is whatever method that they use to remove the gut microbiome may have been more effective than other methods that have been done in the past where you're truly kind of wiping out the gut microbiome.
The problem with antibiotics and antiseptics is that they do kill bacteria. But what ends up happening or what can end up happening is that the most resistant and sometimes the most pathogenic strains are still present just in smaller amounts, so they end up growing back. And we see that with oral health and the use of antibiotics there where a lot of patients are prescribed something like a chlorhexidine mouth rinse to treat oral thrush, and they will take it for a few weeks, their symptoms subside. And then a few weeks later, it flares back up, because you haven't completely wiped out that pathogenic bacteria. So, if you're not making other changes, of course, it's going to grow back. I would need to look at the study, but I guess our definition of wiping the slate clean is it's a spectrum. And I think that there is potential if you truly are starting from baseline and rebuilding from there were probiotics and other interventions might be more effective. Or you might naturally be able to rebuild it if there's some behavioral changes alongside it. But I also think that there's a lot of danger where you can wipe the slate clean, and if you don't make any actual changes, you're giving a chance for those pathogenic bacteria to be reintroduced and grow. Or you're not wiping the slate entirely clean, so you are kind of already starting from a bad state.
Melanie Avalon: Okay, gotcha. Yeah, I will track down the studies and put them in the show notes and also send it to you. I briefly just googled it, and one did come up, but I don't think this was it, because the title of this is "Post antibiotic gut mucosal microbiome reconstitution is impaired by probiotics and improved by fecal transplant." I don't think the one I read was talking about fecal transplants. Or it might have been. In any case, I will find out.
Danny Grannick: I will read it later.
Melanie Avalon: Yeah. When I read it later, I'll know if it was the one I was thinking of. Another huge question that I have is, are there oral probiotics or oral strains, are they in our food at all? Like when we eat fermented food? For example, we know some of those appear in the gut. Does that happen with the mouth or is it not related to the food?
Danny Grannick: There are overlaps. But like, first of all, there's overlaps between the probiotics that you find in a lot of fermented foods. I can't remember the names of the specific companies but there's that yogurty drink that has probiotics in it. So, there's some overlap in the species and strains in those products that are beneficial to both the gut and the mouth. Other probiotics may be different. It really depends on what you're eating.
Melanie Avalon: Okay, gotcha. And trying to say which direction to go, because I do have questions about diet in general. But maybe before that, I mentioned earlier that I had a question about cavities. Before that, broad question, you've mentioned a lot of mouth issues. So, bad breath, cavities, periodontitis. How do these all relate? And what I mean by that is, are some of them actual "diseases"? Are some of them just a state created by bacteria that's not necessarily a disease per se? Like bad breath, is that always something wrong or is that maybe just a side effect that's benign from a health perspective?
Danny Grannick: Yeah, that's a really good question. There's no one answer. I'll start with this. I think this has been an evolution in medical care. And I think it will be coming to dental care and oral health, but the way that we have traditionally characterized and classified diseases has been based on the presence and the severity of associated physical symptoms. So, in oncology, breast cancer was diagnosed as breast cancer because you had cancer in your breast. And it wasn't until we had a really good molecular understanding of what was going on that we are now able to define disease by the mutations that drove the formation of that tumor. And that opened up this whole world of precision diagnostics and precision therapeutics that can be applied to specifically treat those targets.
So, when we think about the diagnosis of a cavity, the literal diagnosis of a cavity is the decay in your tooth. So, it is purely the presence and severity of that physical symptom, but we need to shift the way that we diagnose conditions to focus on root cause because a cavity can emerge from pathogenic bacteria that produce acid and the acid erodes the enamel around the tooth and eventually makes its way to the teeth itself and then you get an answer and you find out you have a cavity. Cavities can also be spurred by mechanical mechanisms. So, grinding your teeth at night, and you can physically wear down the enamel on your tooth and cause decay. And, if you combine that with highly acidic foods or other factors, then of course, you're going to end up with a cavity.
Periodontal diseases, the same thing it's been diagnosed and characterized based on a couple different factors like bleeding on probing is one, pocket depth is another. But it all boils down to, again, physical symptoms, when in reality, at least what we find is there's a very big difference between-- it's a bit more complex than I'm making it but there's a difference between periodontal disease that is rooted in an overabundance of P. gingivalis, than periodontal disease that's rooted in an overabundance of F. nucleatum. It's not one species causes one disease. There's a lot of other things going on there, but we need to shift the way that we diagnose and characterize disease to focus on root cause instead of the outcome of that root cause.
And I think that's been a huge mess in oral care, because if we treat all periodontal disease the same, then we're only going to use-- we're going to use the same interventions, the same procedures to treat it, which is what we've been doing. But the reality is that those procedures are probably somewhat effective for everybody, but they're not really effective for anybody. And that's what we have to shift, to this idea of personalized diagnosis and precision care. And that's what we're trying to do at Bristle. I don't know if that answered your question.
Melanie Avalon: It does and with periodontal disease, just to actually add a definition to it, what do people experience when they have periodontal disease?
Danny Grannick: Yeah, traditionally, it's early periodontal disease kind of the condition associated with it, and maybe touching on your halitosis piece. Gingivitis is technically an early sign or a symptom of periodontal disease. And then, you go through various stages, where stage 1 and 2 have varying levels of pocket depth, I think, you get up to-- Pocket depth for background is defined as the size of the gap between your tooth and your gum line, and it's measured in millimeters. And I may be off on the specific numbers, but the idea is that level 1 and 2, so it's just going up from gingivitis, those are the early stages of periodontal disease, and maybe your pocket depth is 2 to 4 mm or something like that. And then, you go to stage 3 and stage 4. And there's obviously more severe conditions associated with it, where you may have bone loss in a pocket depth of 6 mm. And that's how we've been diagnosing the various stages of periodontal disease up until now.
Melanie Avalon: Is the pocket gap related to receding gums or is that different?
Danny Grannick: Yeah, it has to do with gum inflammation and then gum recession.
Melanie Avalon: Okay.
Danny Grannick: Yeah, it's kind of the outcome of those mechanisms.
Melanie Avalon: And those stages, is it reversible up into a certain point and then not, or how does that work?
Danny Grannick: Yeah, for periodontal disease, I believe, again, up until stage 2, it's generally reversible or you can at least stop progression. And then at stage 3 and stage 4, I believe it becomes a permanent and chronic condition. A lot of our users are in stage 3 and stage 4. And that is where you have to go into the periodontist every three months to again get-- well, I won't get too in depth, but very invasive and very expensive recurring procedures.
Melanie Avalon: Oh, wow. The reason I was thinking about the cavities and was asking that question, this is something that's haunted me for a very long time, which is that I don't remember having a lot of cavities growing up. I'm sure I did, but I don't remember it being a big part of my life. And then, when I did a low-carb diet for quite a while, I had great teeth, like it was great. Then I switched to-- and this was a wholefoods-based diet. And then I switched to a very high carb, low fat wholefoods diet. I was eating and still am eating high protein, a ton of fruit, like a ton of fruit every night and a one meal a day type situation. And when I made that switch, so metabolically, health wise, everything was great, stay the same, something's probably even improved. But I started getting cavities, like so many cavities, and I grind my teeth really bad. And I started getting-- it was bad with my teeth as far as like grinding my teeth away. So, I've been fascinated by the whole concept because I got a lot of cavities but it's a situation where, I don't know if it's because I have a root cause health issue or if it's just because I eat a lot of fruit. And that's just like, what's going to happen with that? So, I guess the question there is do cavities-- And maybe you already answered this as well but do they always indicate a health issue? Like vegans, I feel often have problems with their teeth.
Danny Grannick: Yeah, I would say most of the time, it indicates a health issue like it is the downstream effect of some kind of biological root cause. But other times, it is purely like a physical issue like teeth grinding where the weight-- you're not going to-- you wouldn't take a probiotic if what's actually causing your decay is a physical habit. I mean, maybe you get some other health benefits but theoretically, there's no S. mutans that you have to eliminate, that's going to reduce the incidence of cavities. What's actually causing it as you're grinding your teeth at night, what would really be effective is a mouth guard. And I think that's where we need to start, thinking of the way that we diagnose disease today as actual disease, we need to actually think about it as symptoms and diagnose disease based on the root cause. So, your cavities shouldn't just be called cavities as this umbrella condition. It should be as, an example, bacterially driven cavities or mechanically driven cavities, and there should be a very specific care path that's associated with either one of those outcomes that you can implement.
I think in your case, it may be a combination of the two where maybe the fruits that you're eating are introducing sugar into your mouth, and you may have some caries-causing bacteria that are lowering the pH, creating a more acidic environment. So, that in combination with grinding your teeth is kind of worsening the effect. But again, it's important to understand that as important as it is to identify the bacteria that are causing the cavities, it's equally insightful to find out that you don't have the bacteria that are causing cavities, because that points you in the right direction of what's causing it. And it also points you in the right direction of what changes you should make to address that.
Melanie Avalon: Hmm. Here's a clarifying question to that. For example, could one person be eating a ton of fruit, but for whatever reason, they don't get the type of bacteria that would eat the sugars and create the acid and create the cavities. And then, another person would eat a lot of fruit and would experience that or is it if you're eating a lot of fruit, you're probably going to encourage that type of bacteria?
Danny Grannick: If the bacteria is there and you're eating a lot of fruit-- if you have two people, and they both have the same abundance of the same kind of caries-causing bacteria, and they're eating the same amount of fruit and theoretically, the same amount of acid is going to be produced in their mouth. So, there are some differences in terms of maybe one person is more intelligent about oral hygiene, they use some kind of supplement that helps offset the low pH, so they're lowering their own risk. But at the end of the day, if the bacteria are there, they all function basically the same way. And there may be some genetic differences where maybe one person has stronger enamel than the other person, which mitigates the progression and severity of the symptoms associated with that bacteria, but it's so important to get rid of the bacteria themselves.
Melanie Avalon: I guess what I'm wondering is-- and maybe this is being too black and white, but is it that there are certain strains that would create cavities if they had the right medium? Like, a high fruit diet, for example. And if you had just a little bit of that, but you're not eating a lot of fruit, would they stay dormant? And then, if you eat a lot of fruit-- can you bring out populations that might have been smaller and then once they get whatever they eat, they get bigger?
Danny Grannick: Yeah, so it's like weeds in a garden. Well, maybe, I don't know, I've never really had to deal with weeds in a garden. But the idea is you may have a very low abundance of pathogenic bacteria related to caries, and that population can theoretically be kept in check if you have a bunch of probiotic species of bacteria in your mouth and you're not introducing a lot of sugar. But if you start eating a lot of sugar, those bacteria produce more acid, the acid will shift the pH in your mouth and a more acidic environment is more preferential to caries-causing bacteria. So, you would end up actually decreasing the abundance of some of your commensal species which would give those pathogenic species a chance to expand and replicate, and it's kind of this virtuous cycle of eating sugar, shifting the pH, causing an increase and abundance of caries causing bacteria that In turn produce more acid that lowers the pH further that results in damage to your tooth.
Melanie Avalon: How fast do these bacteria start eating and producing the acid? So, if you have a meal, fruit, or let's even say like a processed sugary meal, while you're eating, are they eating and producing acid? Or if you eat and then immediately-- although I know we should probably talk about this, if you should brush or not right after eating certain foods. Can you stop that before it even happens? Is there a time delay?
Danny Grannick: Yeah, so I think it's probably a bit of both where I would almost think of it is like a grass, where what as you're eating, some of that is being converted by the bacteria in your mouth. But at least the research that I've seen kind of shows that it doesn't pick up until after your meal. I was talking to somebody and their advice early on in the company was-- there was a research study, I'll have to dig it up, but it was basically, most people think that brushing right after a meal is the right to do, but you should actually wait like 30 minutes to an hour and then brush your teeth, because that's the most effective time to do it and mitigate the effects of the bacteria metabolizing whatever foods left in your mouth.
Melanie Avalon: Is that because of the danger of the pH from the food, or is it something else with waiting?
Danny Grannick: I think while you're eating, there's an influx of saliva in your mouth and I think that that helps mitigate like the speed at which they started metabolizing the food. And then obviously, when you're done eating, your salivary production goes down, and the food's kind of sticking around, and it gives the bacteria a chance to start chomping down on it. And then, I think the other piece is-- again, a special kind of cheese is a great example. And one of our advisors, Mark, he is more against Cheez-Its than anybody I've ever met, but for good reasons. Cheez-Its are a carbohydrate-rich food and it's also really sticky. Or we can think about like gummy bears is another good example, where after you're done eating, anybody who has eaten Cheez-Its, you know that there's still remnants of, I don't want to get too graphic here, Cheez-Its in your mouth. And those Cheez-Its happen to stick to places where a lot of pathogenic bacteria like to reside. So, if you don't brush your teeth, and that food's just sitting there, the bacteria are going to continue to eat it and probably replicate and grow in abundance. And then if you wait a little bit, as you're eating, there's food moving through your mouth, I think there's a lot of stuff going on with the saliva. But if you wait a little bit, I think you can dislodge a lot of that food, when it's had a chance to settle.
Melanie Avalon: And while we're in the diet sphere, I've been so fascinated hearing about the role of nitrates and nitrosamines and nitrites, and how the oral microbiome interacts with that. Is that something that you've studied?
Danny Grannick: Yeah, we're actively looking into that, along with a few other things. The idea is, and I don't quote me on this-- you might know actually but I think I was reading this paper. And the paper was saying that the human body doesn't naturally reduce nitrate into nitric oxide. It's a microbial mechanism. But the idea is that nitric oxide is associated with lower blood pressure status. And a lot of the bacteria that perform this mechanism of reducing nitrate to nitric oxide are in the oral microbiome, or at least they should be. And there have been studies showing the association again between poor oral health status and increased risk for cardiovascular disease. So, we've been looking at the connections between the relative abundance of those species and the incidence of high and low blood pressure.s
Melanie Avalon: Yeah, I'm really fascinated and I'm really excited to see the growing information on that because people talk about it a lot and foods for it, and like I mentioned, beats. But the connection between how you mentioned, it's actually the microbes that make that conversion. And I think it's also what determines if it becomes nitrosamine, which is actually not beneficial for health versus nitric oxide. So, I'll be really curious to see what gets developed there with research. When people sign up for Bristle and do the whole program, do you ask about dietary habits anywhere? Are you guys looking at that?
Danny Grannick: Yeah, we do. And we're constantly expanding the questions that we ask. We're making a bunch of updates in the product right now. I think a lot of it is discovery, and a lot of the research is really around the role of diet and the oral microbiome. It's been obviously a lot. There's been extensive research in the gut microbiome, but for oral health, it's kind of been the same stuff for a really long time, which is sugar causes cavities. And that's pretty much where it stopped. So, the way that our team works is we basically go and carry out a bunch of research for a topic that we're interested in. In this case, we can use diet as an example. We get a bunch of papers together and we start sifting through everything. And maybe we start categorizing it according to dietary interventions, where you might have a stack of research that's associated with introducing foods that are really high in nitrate. And then, you may have another stack of papers that has to do with sugar and carbohydrates, and so on and so forth. We want to go through and make sure that we're making calculated decisions around what we're pursuing next. And we also want to make sure that we're not just bombarding our users with like 500 questions, which it would be ideal for us, but nobody wants to go through that.
And then, we'll start to pick the most likely candidates, and we'll introduce those into the surveys that we provide. And that's going to be a constantly evolving piece where if you're on a subscription, you will see like new questions being introduced when you register your next barcode. And that's because we have new research questions that we're starting to investigate. And the same thing is true with your health history, different kinds of behaviors and hygiene interventions, the whole gamut.
Melanie Avalon: Have you thought about incentivizing it? Having this massive, long survey, and if people fill it out, they get a code for a discount off their next order?
Danny Grannick: I haven't, but that is a fantastic idea.
Melanie Avalon: Because then, people will be reordering, and you'll be getting information.
Danny Grannick: Yeah. So, you will probably see that in a few weeks.
Melanie Avalon: Yes. I'm excited. While we're talking about the studies that you guys have done with the user data that you got, I mentioned earlier just how incredibly impressed I am with the research that you have on your site. And one of the really, really impressive articles was one of the articles that you had on flossing. It talks about how surprisingly, the literature to date isn't overwhelmingly supportive of the connection between flossing and benefits to oral health. But then, you guys went and actually, looked at your data, and you have all of the results of what you guys found. Well, just flossing in general, do you think it's beneficial for oral health? And also, what is that experience like? And how do you go about it when you want to test something, and you're looking at user data? Just what is all of that?
Danny Grannick: Yeah, so first, I would say, I think flossing is probably one of the most effective interventions that you can do to improve your oral health. All of our data points to a reduction almost across the board of pathogenic bacteria and actually an increase in commensals. I think this kind of goes back to the recurring theme in oral health, which is there's a lot of research looking at interventions in oral health status, but there's very little research looking at interventions in oral microbiome status. I think a lot of the early research with regard to flossing and some other things as well is the symptoms may not have shifted as quickly as the researchers thought, or they shifted as quickly as the control or some other thing, but they missed the boat on the bacterial and oral microbiome piece. And that's really important for short term and long-term oral health. So, that was really exciting for us.
And it is kind of this idea that-- I hate to use-- oh my God, I hate to use the term 'contrarian', but I think there is this idea of like challenging the status quo in a good and a bad way, we are able to really ask some simple questions and provide new insights to our users where it is as simple as, we have a blog that looked at whether electric toothbrushes are more effective than manual ones. And again, it's kind of something I think a lot of people make assumptions about and they don't really think about other than what their dentist might say, but nobody's really looked at it at the oral microbiome level, and we were able to uncover some really cool insights there.
And the same thing goes for flossing, your dentist tells you to floss. I think most people hate it. But there's very little information that's conveyed to patients about why it's important and like what the real impact is, let alone a way for them to actually see the improvement over time. And that's been really exciting for us.
Melanie Avalon: What did you find when you looked at the electric toothbrushes? Did you find they were more beneficial?
Danny Grannick: So, that one was actually a little bit more nuanced. I can't remember exactly what all the conclusions were, but we did find distinct differences in the efficacy of electric toothbrushes in age groups. I think that we found differences in the efficacy in indication. So, don't quote me on this, but I think we found that it was more effective in reducing halitosis, but we found that it wasn't as effective in reducing some of the species associated with caries or vice versa. So, there were a couple of factors that kind of indicated whether or not an electric toothbrush would be more effective, not generally but like for you as a person. Whereas flossing, there were some nuanced differences, but it was a lot more kind of universal.
Melanie Avalon: With electric toothbrushes, if I had to guess, I would hypothesize that they would be more beneficial in young kids. Do you look at that?
Danny Grannick: No, we haven't.
Melanie Avalon: I don't know. But because kids are the ones that are not going to be putting in effort for brushing. So, I feel they would might benefit more from a little help, compared to an adult who might put more effort into their brushing.
Danny Grannick: Yeah, I'm looking at-- Yeah. Children's oral health is kind of this whole other world that we haven't been able to do as much work as we want to in, but we certainly intend to. I'm looking at the blog article, and it looks like people under 30 had higher commensal scores when using an electric toothbrush versus those using a manual one. We also looked at brushing frequency with them. If you use an electric toothbrush, that's great. But are you actually brushing like two or three times a day or are you only doing it once? So, we found that, let's see, people using either manual and electric toothbrushes had similar commensal scores, but people who brush twice per day and used an electric toothbrush had significantly better commensal scores than those using a manual one.
Melanie Avalon: Oh, wow. And what you have to wonder though also is causation correlation. Are the people who are going that intense with their habits, or they also doing all of these other oral health habits?
Danny Grannick: Yeah, that's why it's important to look at-- That's why data is the big piece. It's the same reason why we did the shotgun metagenomics approach versus something else, because you can make a lot of assumptions where, yeah, I would imagine that somebody who invests $300 in their Oral B electric toothbrush is probably a bit more diligent than somebody who's buying like the $1 toothbrush at Rite Aid. Or somebody who's replacing their toothbrush every three months probably has better habits than somebody who doesn't for years. So that's why it's important to not only just look at the surface level but start to tease out the assumptions that people might start making where somebody who has an electric toothbrush invested more, so we would expect them to brush more times per day, because they are better about oral hygiene. So, we really want to try to get as close to base truth as possible.
Melanie Avalon: Speaking of the replacing, how often do you recommend replacing your toothbrush? That's something I've had a big change in because I used to replace it-- I don't even know, maybe once a month. But then I had a moment. And this is not super sustainable for the planet. But I realized I was like; toothbrushes aren't that expensive. I could be replacing it a lot and feel cleaner. But I don't know if that's just in my head. I don't know if I actually need to be replacing it as much as I do. Do you have thoughts on replacing toothbrushes?
Danny Grannick: Definitely do it. There's a whole host of reasons. I would say at a minimum, replace it every three months. We're doing some research there as well. One, your toothbrush is just sitting there and--
Melanie Avalon: In the bathroom, where you're flushing the toilet. I don't know [laughs].
Danny Grannick: Yeah. So, for one, your toothbrush is just kind of sitting out there and it's wet. And you can imagine that-- you wouldn't leave your cup with water in it for a day and just keep refilling the same cup without ever washing it. So, I don't know why we do that with our toothbrush. But the other piece is, yeah, it's in your bathroom and your bathroom isn't exactly known for being the most sterile place on the planet. There was a study done a while back that had showed there were-- this is going to be graphic, but they were looking at flushing and the dispersion of fecal particles. And I think found-- yeah, I think they found that if you leave your toilet seat open and you flush that fecal particles disperse, I think it was something like six feet around your toilet. So, I'll let the audience kind of draw their own implications from that. But yes, I would replace your toothbrush.
Melanie Avalon: I saw something about that forever ago, like years and years ago, and it has stuck with me to this day. And I'm crazy, like I mentioned replacing a lot. I replace my toothbrush probably every two weeks. But I just feel cleaner.
Danny Grannick: Yeah, I think the more often the better. Yeah.
Melanie Avalon: I should probably-- that's something else I should create-- like a toothbrush that's really sustainable. I know there are some sustainable options, but I haven't found one that I super love. So, question about the recommendations and actually I guess I can look at my results so listeners can get an idea of what happens when they do the whole process. I got back my results and what's super cool is it gives you results and then you get your own score and then you get it how you compare to healthy people.
So, beneficial bacteria, I got moderate. I got 5.5/10. So, the ideal healthy people is 10. I got 5.5, which was not super exciting, but then you get more information about it says how it relates and the strains that might be related to that. Out of curiosity, I don't know if this is information that you can give, how many people have done Bristle? If you can't say, that's fine. I'm just wondering how many people you're comparing to.
Danny Grannick: Yeah, unfortunately, I can't, but I can say that data that we're comparing in those graphs isn't actually consumers. We are launching a feature for that, but we want it to be as again as close to ground truth as possible. So, the data that you're looking at is actually from the clinical research study, and it's all de-identified more as an aggregate. But when we talk about healthy patients, those are healthy people. Those were patients that were diagnosed as being healthy in the dental clinic. And same thing for the gum inflammation score, those patients who are comparing you to are patients who are diagnosed with periodontal disease.
Melanie Avalon: Okay. Yeah, for gum inflammation, for example, I also got moderate, I got 4.4. So, people with gum inflammation, it says are 10 and then healthy people without gum inflammation, it compares to 2.2. Interestingly, well, for halitosis, bad breath, I got low. So, that made me happy. For tooth decay, I got undetected, how common is that, that you have undetected bacteria?
Danny Grannick: Yeah, it's more common than I thought it would be. The bacteria that cause cavities are by nature-- if we're looking at the oral microbiome as like a pie chart, even people with a higher score have still contextually a very small abundance of caries causing bacteria. The effects of those bacteria, I think, are just more severe. We do get undetected quite a bit, more often than I thought we would, which is interesting, but it also kind of suggests that the mechanical piece of cavities is more prevalent than we would have thought. And generally, I think my caries, opening up my results, but something like 0.2, because usually there is some abundance of carriers causing bacteria, but we do get plenty of people that get zeros.
Melanie Avalon: That's so interesting, especially given I mentioned my history, I've had a lot of dental work done because of how much I grind my teeth. And also, I've had veneers. So, it's really interesting to see that effect.
Danny Grannick: Yeah. One of the other pieces, and we were kind of talking about this earlier, is the way that we diagnose cavities. You can have a lot of cavities, but it doesn't necessarily mean that they were brought on by pathogenic bacteria. And in certain cases, there's something called incipient caries. And it's basically like you had a cavity and they were able to stop the progression of that cavity. But sometimes, whether or not that cavity is diagnosed is up to the dentist. So, sometimes you'll get very conservative dentists that are mitigating early risk where they recognize like, "Hey, this is an incipient cavity and we should do a filling just to make sure that it's all good," even though it's not progressing, it's not getting worse, and you may not even have bacteria that are contributing to it. Whereas other dentists may be a bit more liberal, and don't formally diagnose it as a cavity yet until it continues to progress. So sometimes, the lens that people are looking at your mouth through can influence your diagnosis.
Melanie Avalon: That is something I've wondered. Getting a filling, are there any downsides to that? Is that only helpful? Have a negative effect on your mouth?
Danny Grannick: I don't think it will have-- well, there are some downstream correlations that people are looking into with regard to cavity fillings and root canals and things like that. But in terms of treating the decay that is present, again, if we ignore kind of the microbial aspect, and we just looked at look at it as a physical symptom that's present, then doing a cavity filling makes sense, because you literally have a hole in your tooth and that hole needs to get filled. I think there's other situations that fall into shades of grey, where early caries is preventable, and it is reversible. And some dentists will instead defer to a cavity filling rather than implementing behavioral change and vice versa. So, there are gray areas for whether or not those procedures are medically necessary.
Melanie Avalon: Yeah, it's interesting. When I was really experiencing issues with my mouth, the dentists that I saw said was that it was probably mechanical because all of my issues were on the bottom of my mouth and nothing on the top. And she was saying that if it was related to a bacteria issue, then I probably would have seen it all throughout my mouth, not just on my bottom, but probably was from grinding. So very, very fascinating. Okay, and then I keep mentioning the recommendations. When you do the Bristle program, you get recommendations. And first question, I was given seven recommendations, and I can talk a little bit about them. But before that, how many total recommendations are you pulling from? And how customized is it to the individual?
Danny Grannick: Yeah, right now, the recommendations are mainly around products. In the next couple of weeks, you'll see that expanded to diet and hygiene recommendations as well. So, you'll have even more stuff to sift through. We also right now include alternatives, and I think this will probably open up another conversation. But you might see like fluoride and nanohydroxyapatite listed. Those ingredients aren't normally both found in the same toothpaste. Usually, you can find fluoride-based toothpaste, or you can find hydroxyapatite-based toothpaste. So, we're building in logic as you take your survey that includes like preferences for what kinds of ingredients you may or may not want. And that'll become-- there will be more recommendations, but there'll be more targeted recommendations. And we're constantly evolving the logic between the products, diet, and hygiene recommendations that we make in your oral microbiome. Right now, it is connected to your actual results. So, there are products that will show based on specific bacteria that are in high abundance or low abundance, are present or not present, as well as your high-level scores.
Melanie Avalon: If listeners are curious, you get like the name-- I actually didn't get either of those. I didn't get fluoride, or-- I never know how to say it. It's that hydroxy--? What is it, that other one?
Danny Grannick: Nanohydroxyapatite, it's a mouthful. I guess [unintelligible 01:21:56] fun. I have to use that more.
Melanie Avalon: Well, it's funny because it's like a thing that people are looking for as an ingredient, but it's such a long word that I never remember what it is. So, like an example I got is-- what's one that I can pronounce? Chlorine dioxide, and then you click on it, and it says what it does and how it works. And then, it gives you names of specific brands that it's in. One of them I'd used before, Closys, and then it gives you references. So, it's very, very helpful. My listeners, I know will be really upset with me if I don't ask you the question. You mentioned fluoride. What do you guys think about fluoride? Because I know that can be very polarizing, especially in the more holistic health world.
Danny Grannick: Thinking about myself two and a half years ago before we started the company, never imagined that I would be having as many conversations about fluoride as I have today. My most objective opinion is we need more evidence. I guess what I'm saying is there is clear research that shows that fluoride is an effective intervention for the prevention of caries. If we're talking about just cavities, and protecting yourself and mitigating risk for cavities, fluoride has been shown to be effective. There's obviously been a lot of research showing that it is also implied in some neurological conditions. What I think we're really lacking is like a full-scale study, a longitudinal study with an adequate sample size and very rigid criteria that looks at the effect of fluoride long term. And again, I don't fall necessarily on either side of the debate and neither does Bristle, because, again, we are trying to be as evidence based as possible. And right now, we make the recommendation for two reasons. One, we are constantly looking at the evidence behind it. And as soon as we find the right kind of data and the right kind of evidence that truly indicates that it is harmful, of course, we would remove it as a recommendation. And we've proactively done that with other ingredients in the past, like chlorhexidine.
We also include it because for a lot of people, fluoride is an accessible intervention. Right now, I think nanohydroxyapatite tends to be this higher end ingredient that's included in a lot of premium brands. And that's not to say that it's not more effective. It has been shown to be equally effective in the prevention of caries as fluoride. So, that's why we list it as an alternative. But at the same time, you know, not everybody can afford premium brands. And some people really only have access to a Walmart or CVS or something that that limits their selection. So, we do want to make sure that people are adopting changes that they can actually implement. And that's one reason that we include fluoride.
Yeah, it's very debated. I think one nuance in a lot of the research is that the data showing the neurological effects has largely been attributed to the continuous and acute ingestion of fluoride. There's-- what's the saying? Everything's okay in moderation or something like that. Right now, we live in a society where our water is fluoridated, our toothpaste is fluoridated, everything in a dental office is fluoridated. Like, it's a lot of fluoride that were in taking, especially if you're drinking water straight out of the tap, and you're using a fluoride-based toothpaste and you're to some degree ingesting all of that. There have been studies that have shown that topical fluoride use does not produce the same effects. So, again, just using a fluoride toothpaste to brush your teeth and spit it out into the sink may not be as damaging as ingesting fluoride continuously for years. All that to say, I think that there's more research that has to be done, and we're certainly looking into it as a company. But we don't want to close that off as an option for anybody right now until we know more.
Melanie Avalon: Well, yeah, it's interesting, because I have not used fluoride product-- I haven't drunk fluoridated water, and I have not used fluoride and my toothpaste for probably like a decade. And every time I would go into the dentist with these cavities that I started getting after the high fruit diet, every time I would get schooled about how I needed to be using fluoride in my toothpaste, and I wonder a few things. One, I wonder if I had been doing that, if maybe I wouldn't have had all the issues that I had, if it would have been protective? Two, I also wonder, the effects of fluoride, is it from the fluoride literally touching your teeth, or systemically does it have the benefit? So, when we're drinking the water, is it just from the fluoridated water touching the teeth? Or do we get it because we're drinking it and it's in our system, and then it also goes back to our teeth from drinking it later?
Danny Grannick: I know that part of it is the introduction of fluoride directly to the oral environment, which is why we have fluoride in toothpaste. I believe that there is a mechanism for just increasing systemic fluoride and having that reintroduced through your saliva into the oral cavity. But I think the other piece here that a lot of people are missing is fluoride is a preventive intervention, but I think it's also quite reactive. You can eliminate fluoride from everything that you use if you're also changing your behavior and changing your diet. You can brush with water, because you're still removing a lot of those pathogenic bacteria and the plaque from your teeth. The fluoride does help remineralize enamel and protects the tooth from the effects of acid, but decreasing the production of acid by addressing the bacteria that produce it is a totally viable and non-fluoridated path that anybody can take as well.
Melanie Avalon: Okay, I think that's a very measured answer. I guess just for me personally, I wonder, maybe I should have been doing like just topical fluoride and maybe [unintelligible 01:28:07] effects?
Danny Grannick: Yeah, nanohydroxyapatite has been shown to be as effective. So, you can use either.
Melanie Avalon: The problem with that, when I was looking it up was, I wasn't able to find a brand I liked the ingredients that had that. But I should do another look for it, which speaking of-- I ran my entire routine by one of your experts, Evan, is that her name?
Danny Grannick: Eman.
Melanie Avalon: Eman. I should know this, I follow her on Instagram, and she was fabulous. But something that's so cool about Bristle is you have the opportunity to actually have a phone call with an expert who helps go over your results and can give you thoughts on your personal routine. And she even sent me like a recap of recommendations. And I was really blown away by that personal touch and what I learned from it, especially because I think-- it's so incredible, just in the entirety of health, the advances that we're making, and so much data that the everyday user can get regarding their health. So, be it blood tests, be it the gut microbiome, now the oral microbiome. But it can also be a little bit of overwhelmed with data, and it's also trusting that the consumer has the knowledge base to form the correct conclusions from all of that.
So, it can be very overwhelming. And you guys have done a really-- I mean a really amazing job and making the results that the individual user gets, making it user friendly, making it very clear. And at the same time, it can get very detailed. So, basically you can get your results and you can learn as much as you want to learn or if you just want surface-level basic recommendations, you can just look at that. But then on top of that, to have that one-on-one interaction was really amazing. So, I applaud you for that. And I really, really encourage listeners to try this out because it is so eye opening. I know we talked about this before, how you're changing and enhancing that whole program, but what does the future look like for Bristle? What do you hope to achieve and accomplish and see and the user experience, h ow might it be changing? What are you looking for now?
Danny Grannick: Yeah, at the highest level, we as a company, we think that oral health has been this overlooked but critical component of overall health. And our goal as a company is to help people improve their oral health to improve their overall health. Our bet is by helping people rebalance their oral microbiome will not only decrease or eliminate the prevalence of oral disease, but we'll see a reduction or an impact in the prevalence of diabetes, cardiovascular disease, cognitive decline. So, that's kind of the big vision for the company.
But in terms of what we want to do on the product side, I think oral health is just such a black box right now. We never know what our oral health statuses. We only find out that we have disease when it's progressed to the point where we need an expensive or an invasive intervention. And we want Bristle to be a more effective and more accessible standard of care for people. More effective in the sense of detecting disease earlier, being more precise about the way we characterize it, implementing behavioral preventive recommendations across the diet, hygiene, and the right products to use for the bacteria that you have and the oral health status that you're at.
And accessible in the sense of-- one of the statistics that really stood out to me, when we were doing initial research around Bristle, was 80 million US adults skip dental checkups every year, which isn't, I guess, it's not that surprising, probably for a lot of people. But the three most commonly cited reasons were inconvenience, cost, and fear. And what we want to deliver is a more approachable, accessible, easy-to use-experience. And that was a big factor in us going direct to consumer because we didn't want to limit the availability of our technology to people who already saw a dentist or who had access to see a dentist. We want everybody to be able to take-- whether it's your 0 to 1, like first step and oral health, or you're going from like 8 to 10, we want to open the door to everybody.
In terms of the product, we want to be the source of truth, I think, for people to understand their oral health status and to implement really effective changes to improve their oral health, and we want to direct them to the best-in-class products that will have the biggest impact. And we, right now, work with a variety of companies and obviously make referrals to brands that aren't Bristle, and I want to maintain that. I think one of the things I'm most proud of as a company is that we are objective, we aren't trying to just sell people products, because we make them and it's adding to our revenue. We are trying to point people to products, because they're the most effective options that those people can adopt. So, we want to continue working with other oral care product companies to get their products into our recommendations, to test them and understand the effects that certain ingredients have and work with them to create better versions of their products for people. We think that there's probably some opportunities for us to introduce products or at least work with companies to introduce new formulations and new ingredients.
And we also want this to be adopted into the standard of care. Because right now, it is a purely reactive process. And more than anything, I would love to see dentists and hygienists leveraging Bristle as part of their practice to really shift from pure reactive treatment of disease to proactively managing health, a more consultative standard of care with their patients.
Melanie Avalon: That is amazing. And that was one of my initial thoughts when I experienced Bristle. Because I work and I have interacted with and engaged with a lot of, not oral microbiome, but brands like this where there's a test and then you learn something and then there's product recommendations. And so often, it does feel-- oftentimes it is very helpful, but it also feels like the purpose is to be a funnel towards a product run by the company. When I saw Bristle, which I know-- right now, you guys don't have any products right now, right?
Danny Grannick: No.
Melanie Avalon: I would anticipate I would hope that you guys would hopefully in the future because then we would-- I mean especially after talking to you now, I just really trust where you're coming from with any products that you would create. But like I mentioned, it's very cool that in the recommendations you list out all of these different brands and it comes off as just completely unbiased, which is really refreshing. It's kind of like the best of both worlds because I didn't realize this, but it is HSA, FSA eligible. So, does that mean that we can use our HSA account card to purchase the kits?
Danny Grannick: Yes.
Melanie Avalon: How often do you recommend-- Because it's cheaper, the more you test per year? How often do you recommend people be testing and retesting?
Danny Grannick: Yeah, I think for most people, every six months is kind of the baseline that we've seen. We're starting to do more testing with more frequent tests. But I would say the majority of people on the six-month testing plan are probably in the right place. Of course, you can always start with the single kit just to get a snapshot of your oral health status, and then determine things from there. The three months, I think, is very effective, especially if you're really invested in your health. And like we talked about, the oral microbiome is really dynamic. Your oral health does shift and the recommendations that we make change as your oral microbiome changes. So, it's just another way to kind of stay on top of things and make the changes that you need to make to address whatever risk you have at any given time.
Melanie Avalon: Awesome. Well, we do have a code for listeners. So, thank you so much for this. Oh, out of curiosity, do you know if my code is good on subscriptions, or is it just the one-time purchase, for the initial?
Danny Grannick: We'll make it good for the subscriptions. If it's not, I'll email somebody after the call and make it so.
Melanie Avalon: Thank you. That's amazing. If you go to melanieavalon.com/bristle, that's B-R-I-S-T-L-E, that will redirect to their landing page for me on their website. And you can use the coupon code, MELANIEAVALON, to get 15% off. I am so grateful. Thank you for that. I am really excited. I just had such an amazing time doing this. Like I said, it was something I thought was really important, and it's thrilling to see a company actually tackling this in such a broad way. I mean, with the research, with the empowerment of consumers to actually learn about their health, and then all of the information that you provide is just so cool, so important. I cannot recommend it enough. I can't wait to hear from listeners what they experience.
So yes, well, we covered so much information. The last question I always ask every single guest on this show, and it's just because I realized more and more each day how important mindset is, what is something that you're grateful for?
Danny Grannick: Yeah, I want to say, obviously, the team and the company and our users have all been great. I think that's a really unique situation for me to be in. Honestly, I started the company in San Francisco, and San Francisco is an amazing city. I moved back to San Diego, where I'm originally from, 10 or 11 months ago. And a big component of that was the mental health piece. I think there's been a lot of advantages from a mental health perspective of just being in a place that's a bit slower paced, not being kind of surrounded by "scene" of tech and startups and investors. It's allowed me to focus on the mission a lot more and connect with our users. And I think on the other end of the spectrum, I grew up surfing, and that's always been like my personal outlet.
And I would say I'm just grateful-- It's so rare. And I don't think about it enough. I'm glad that you brought the question up. But it's such a cool opportunity for me, and I feel so grateful to be able to build a company that I believe in and do it in a place that I enjoy being and still having time in my life to do the other things that I love. Having access to the ocean and being able to surf, it's another thing that like very few people get to experience. And I think a lot of the time, I take a lot of these things for granted and you just get so granular in the day to day of running the company and building things. But yeah, I'm really grateful for where I live right now and the fact that I do have time to go do those things.
I'm grateful for my girlfriend who's been incredibly supportive and was there from the beginning of the company. Her name's Nicole. I got a puppy a few months ago. Her name is Lola. So, that's been kind of the light of my life for the last couple of months, and she's been great. I'm grateful that she's been an easy puppy because that could have made my life a lot more difficult. Yeah.
Melanie Avalon: Well, that is amazing, and not to end on a crazy rabbit hole, but my interview tomorrow actually it's with Dr. Karen Becker, who wrote a book called The Forever Dog so it's all about the longevity and dogs and all about their health and how it correlates to human health. I don't think she talks at all about the oral microbiome of dogs. That might have to be something you look into in the future.
Danny Grannick: Yeah, there's some really interesting-- there's a lot of research into the overall microbiome of dogs and cats actually, some interesting indications there.
Melanie Avalon: Oh, really? Oh, hey, wow. Okay. See? There's just so much here. Well, thank you again. This conversation has been amazing. I am so grateful for what you're doing. I mean, literally, you're changing the world because I don't know anybody else doing this. And I really think this is the beginning of a huge frontier that hopefully will be more and more explored and become more and more accessible, which is something you're doing with Bristle. So, thank you so much. Love to stay in touch and I'm really excited to see the future of everything.
Danny Grannick: Absolutely. Thanks for having me. It was great being here.
Melanie Avalon: Thanks, Danny. Bye.
[Transcript provided by SpeechDocs Podcast Transcription]