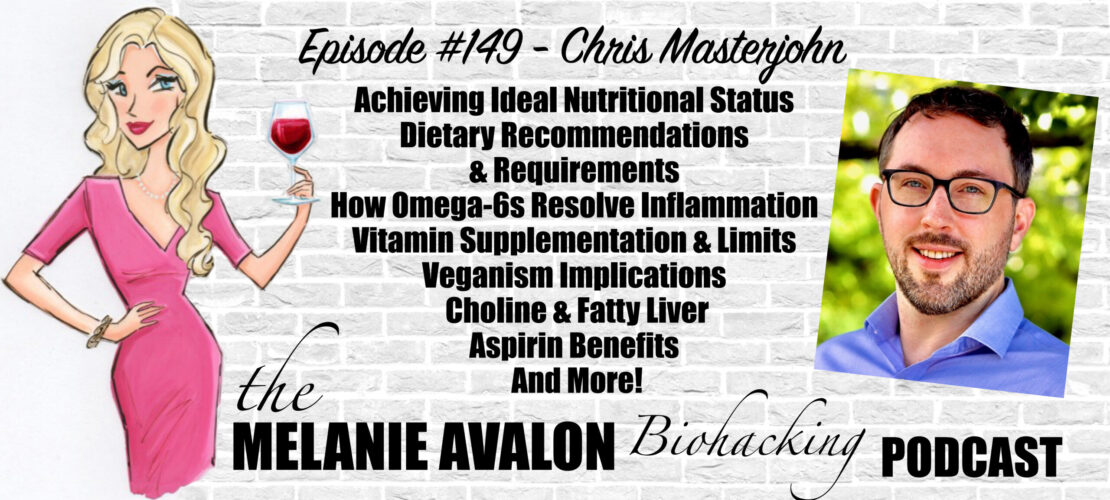
The Melanie Avalon Biohacking Podcast Episode #149 - Chris Masterjohn
In the fall of 2016, I made the decision to leave academia and pursue entrepreneurship a transition I completed on January 1, 2017. If you would like the full story of how I came to this decision, you can join my email newsletter, and the first welcome email tells the story and provides you with my vision going forward.
As of January 2017, I'm on my own. I am currently conducting independent research, consulting, working on information products, collaborating on information and technology products, and producing tons of free content to help people gain better health.
I have deep and personal experiences with the power of food, movement, and mindfulness to support health and well being. I want to take what I've learned and pay it forward.
But I'm not done learning. I'm constantly learning from my own challenges, failures, and successes, and I'm constantly learning by scouring the scientific literature, whether I'm uncovering long-forgotten and neglected evidence from yesteryear or following and deciphering the latest findings.
What I try to do here is grapple with complex science and translate it into practical principles that each of us can use to better support our health.
LEARN MORE AT:
chrismasterjohnphd.com
@chrismasterjohn
SHOWNOTES
2:25 - IF Biohackers: Intermittent Fasting + Real Foods + Life: Join Melanie's Facebook Group For A Weekly Episode GIVEAWAY, And To Discuss And Learn About All Things Biohacking! All Conversations Welcome!
2:40 - Follow Melanie On Instagram To See The Latest Moments, Products, And #AllTheThings! @MelanieAvalon
3:10 - AvalonX Serrapeptase: Get Melanie’s Serrapeptase Supplement: A Proteolytic Enzyme Which May Help Clear Sinuses And Brain Fog, Reduce Allergies, Support A Healthy Inflammatory State, Enhance Wound Healing, Break Down Fatty Deposits And Amyloid Plaque, Supercharge Your Fast, And More!
AvalonX Supplements Are Free Of Toxic Fillers And Common Allergens (Including Wheat, Rice, Gluten, Dairy, Shellfish, Nuts, Soy, Eggs, And Yeast), Tested To Be Free Of Heavy Metals And Mold, And Triple Tested For Purity And Potency. Order At avalonx.us, And Get On The Email List To Stay Up To Date With All The Special Offers And News About Melanie's New Supplements At avalonx.us/emaillist, And Use The Code MelanieAvalon For 10% On Any Order At avalonx.us And mdlogichealth.com!
6:40 - FOOD SENSE GUIDE: Get Melanie's App To Tackle Your Food Sensitivities! Food Sense Includes A Searchable Catalogue Of 300+ Foods, Revealing Their Gluten, FODMAP, Lectin, Histamine, Amine, Glutamate, Oxalate, Salicylate, Sulfite, And Thiol Status. Food Sense Also Includes Compound Overviews, Reactions To Look For, Lists Of Foods High And Low In Them, The Ability To Create Your Own Personal Lists, And More!
7:15 - BEAUTYCOUNTER: Non-Toxic Beauty Products Tested For Heavy Metals, Which Support Skin Health And Look Amazing! Shop At Beautycounter.Com/MelanieAvalon For Something Magical! For Exclusive Offers And Discounts, And More On The Science Of Skincare, Get On Melanie's Private Beautycounter Email List At MelanieAvalon.Com/CleanBeauty! Find Your Perfect Beautycounter Products With Melanie's Quiz: Melanieavalon.Com/Beautycounterquiz
Join Melanie's Facebook Group Clean Beauty And Safe Skincare With Melanie Avalon To Discuss And Learn About All The Things Clean Beauty, Beautycounter And Safe Skincare!
12:30 - Chris' Start in Nutrition
17:20 - weston price's principals
26:25 - LMNT: For Fasting Or Low-Carb Diets Electrolytes Are Key For Relieving Hunger, Cramps, Headaches, Tiredness, And Dizziness. With No Sugar, Artificial Ingredients, Coloring, And Only 2 Grams Of Carbs Per Packet, Try LMNT For Complete And Total Hydration. For A Limited Time Go To drinklmnt.com/melanieavalon To Get A Sample Pack For Only The Price Of Shipping!
30:15 - veganism
32:30 - longevity with veganism
37:00 - creatine
39:20 - synthesizing vitamins, deficiencies, and RDAs
47:20 - niacin
52:50 - cravings driving food intake
56:00 - supplement toxicity
1:03:30 - liver as a superfood
1:07:30 - a study rats unnatural diet & environment
1:14:15 - DRY FARM WINES: Low Sugar, Low Alcohol, Toxin-Free, Mold-Free, Pesticide-Free, Hang-Over Free Natural Wine! Use The Link DryFarmWines.Com/Melanieavalon To Get A Bottle For A Penny!
1:17:00 - the derangement of the modern Palate
1:22:20 - choline & fatty liver
1:32:00 - is choline production demand driven?
1:32:45 - high dose choline
1:34:40 - polyunsaturated fats, EPA, DHA & inflammation
1:44:00 - the balance of different cell types & wound healing
1:52:30 - resolution of healing
1:54:45 - Omega-3s
1:56:55 - aspirin
1:59:10 - NR vs NMN
TRANSCRIPT
Melanie Avalon: Hi, friends, welcome back to the show. I am so, so incredibly excited about the conversation that I'm about to have. This is one of those guests that when I first decided way back in the day to even start this podcast, I made my list of dream guests. And today's guest was at the very, very top of that list. I'm here with Chris Masterjohn. I have been following his work for years, probably, since around 2014. How long have you been blogging, Chris, on the internet?
Chris Masterjohn: Well, it depends what you mean by blogging. But I've been writing since 2004.
Melanie Avalon: Okay, so, a long time. I know the word blog sounds very casual. This is more than just a blog. But I've been following your work probably since around 2014. What's so, so incredible about Chris' work is he covers pretty much every topic you could ever think of related to health and nutrition, and not surface level. I was actually talking about this because I mentioned to my cohost on The Intermittent Fasting Podcast that I was going to be recording this today. I was thinking about it. Whenever I read about a topic that you write about, somehow, you go into it deeper than anything I've read from anyone else and I always walk away having learned something that nobody else has talked about. It makes so much sense the stuff that you say and I just don't know how this isn't more common knowledge. In any case, I heard you recently on our mutual friend, Robb Wolf's podcast. So, I begged Robb to introduce me and here we are. So, I am just really, really excited.
What's interesting I was saying this before the show is, there're so many topics I just want to pick your brain on. This might just be a rabbit hole of wonderful adventures into science. On your website, you have your bio. You earned your PhD in Nutritional Sciences from the University of Connecticut in 2012. Then you served as a postdoctoral research associate in the Comparative Biosciences Department at the College of Veterinary Medicine at the University of Illinois. Then you were Assistant Professor of Health and Nutrition Sciences at Brooklyn College from 2014 to 2016. But what I love at the very end of your bio is you say, “Please join me in the pursuit of truth, learning, and wonder” and that is just pretty much the most amazing challenge that you can put out there. So, all that to say, I'm very, very excited and thank you so much for being here.
Chris Masterjohn: Thank you for having me. It's a pleasure.
Melanie Avalon: To start things off, I imagine a lot of my listeners are probably very familiar with you. But for those who are not, can you just tell us a little bit about your personal story? Were you always interested in nutrition? Did you have an epiphany one day that made you want to go that route? What led you to doing what you are doing today?
Chris Masterjohn: I think if we go way back, my interest in nutrition was largely influenced by watching my mother's battle with fibromyalgia. She had a phase in her life, where she was just in constant pain, not sleeping at all, because of it. She got involved in a variety of holistic approaches that included macrobiotic diet, and yoga, and herbalism, and all kinds of stuff like that. Whatever it was, she experienced a tremendous amount of healing and achieved a life that was, I don't know if it was completely pain free, but one where she had gotten a normal life back. That was when I was a teenager. I was very interested in alternative health, which included understanding nutrition at that time. Those experiences for her also made her buy a lot of books like, Prescription for Nutritional Healing was an early one. I would flip through them and we had an appreciation of nutrition because of that. My curiosity and self-experimentation led me down a number of different diet-related routes. I was on the Zone Diet for a while, very serious, made that-- that's 40% carb, 30% fat, 30% protein plus fish oil diet. Then I got into veganism. I read a book called Diet for a New America by John Robbins of Baskin and Robbins heritage.
Melanie Avalon: Of Baskin and Robbins.
Chris Masterjohn: Yeah. I'm not sure where he was in the family, but he was one of the Robbins family from Baskin-Robbins. He was the family black sheep that [chuckles] decided that his family fortune was built on poisoning people by feeding them dairy products. [laughs] That book argued that going vegan was basically going to save your own health, as well as the welfare of the animals, and the welfare of the planet. For those three reasons, I went vegan. That eased into it over six months. I was vegetarian for a bit and then vegan-- The vegan phase didn't work out very well for me at all. It was my recovery from that really launched me into the career that I have now. When I was vegan, I developed a number of problems. One was that my teeth fell apart. I did have a high cavity rate when I was a kid. I hadn't gotten a cavity in a long time. By the time I was in my very late teens to early 20s, the vegan period overlapped. I might have been 20 when I was-- I was either 19 or 20. It sort of overlapped the turning of my teenage into 20s. I haven't had a cavity for a long time, but the next time I went to the dentist after I had been vegan, I had over a dozen cavities and I needed two root canals. So, that was a big problem.
Another thing that happened was, I had anxiety disorders that a collection of all the ones you would find in the textbook, but mildly neurotic nuisance levels when I was a teenager and they aggravated to a magnitude to the point where I was probably borderline psychotic when I was vegan. I remember one time one particularly pointing example. I was just completely obsessed with the idea that my food was drugged or poisoned. I was constantly checking for signs of this. I remember one time where I was inspecting my veggie burger. I was inspecting the wrapper for 20 minutes looking for signs of tampering. After some large number of those minutes, I think I had scratched the wrapper. I found my evidence, but I couldn't decide whether I did it or was there the whole time. I was so hungry, and I got really, really angry myself for not being able to eat any food. I just threw the veggie burger across the room at the wall, and then went into my room, and cried.
Many, many things in the story happened that eventually helped me to learn of the work of Weston Price. Weston Price was the first Research Director for what became the American Dental Association for 25 years. Then he became a pioneer in Nutritional Anthropology. He was exploring the world studying traditional diets and the transition of modern diets in the 1920s and 1930s and he was writing in the 1930s or the 1940s about it in a book called Nutrition and Physical Degeneration. He had basically documented, I guess, two principles. One of which I think is not really very surprising or controversial today, which is that as people went from their traditional diets to what he called the displacing foods of modern commerce, white flour, white sugar, white rice, canned-- vegetable oils, syrups, and canned goods, their health dramatically declined. Physical degeneration as he put in that title. He was particularly adept at studying teeth and facial structure. That's where his work really shined was in studying the destruction of the teeth in the first generation, and just the palate, and the facial structure in the second generation on these foods.
I think not that every finding related to that was-- I shouldn't say he didn't call his book, nutrition and tooth decay, because he also developed a lot of evidence, especially when he could talk to doctors that lived with these people and could report on the incidence of other problems. He basically found that the destruction of the teeth and the palate correlated with the dramatic rise in basically all degenerative diseases. He had some pretty good evidence around cancer, and gallbladder problems, and some other issues. He had some moderate level evidence around heart disease. But the principal finding was that when you move on to a diet that is mostly based around white flour, white sugar, and these other displacing foods of modern commerce, your health just completely falls apart. I don't think that would surprise anyone. Most people, just to some degree acknowledge that you can't eat mostly white flour and white sugar.
The other side of that, though, was that he really emphasized that these groups that he was studying on their traditional diets, who were extremely healthy had bodies of wisdom about what to eat built on generations of experience. And that they very much went out of their way to get certain categories of foods that Price-- He decided the important thing that tied these categories together was these foods content and fat-soluble vitamins. He outlined four categories of foods and he said, “Not every group ate all of them, but all these groups went wildly out of their way to procure foods from at least one if not more than one of these categories.” These categories as he grouped them were egg yolks and organ meats in one category. Dairy products, always full fat dairy products in another category. The animal life of the sea, so, fish and especially shellfish in the third category. Then the fourth category was small animals like frogs and insects. Of course, in that fourth category, when you're eating animals that are that small, you are intrinsically eating the whole animal. The same thing is true with—
Generally speaking, all these groups did eat the whole animal anyway, but if you're talking about shellfish, they're not quite wired the way that like walking animal is, but you are eating the whole thing. The presence of whole animal consumption with organ meats and egg yolks in one category, and shellfish in another category, and small animals in another category is really something that's tying these together. I am reading this while I'm on my way out of veganism and I'm realizing that not only was I not eating any of these foods as a vegan, but even most of my omnivorous friends were not eating any of these foods. I would say, in the American diet, the ones that we eat the most of our eggs and dairy, but egg yolks have been shamed from a health perspective for a long time because of their cholesterol content. People don't eat organ meats anymore for the most part. Some people do, but most people don't. Fish and shellfish is very hit or miss. Some people like seafood, and some people don't and, and the average person doesn't eat a lot of seafood. Of course, pretty much no one eats small animals and insects in mainstream society.
I realized that I had gone from a very mediocre, omnivorous diet. Not a good of omnivorous diet to the complete end of that poll of not a great diet in my vegan diet, where I just wasn't eating any of the foods that were in these categories. I rearranged my diet along the principles of Weston Price through specially emphasized nutrient dense animal foods including organ meats. Remember the story that I had told you about the veggie burger. Now, fast forward to a few months into this diet, I find myself in the dining hall where I was a dishwasher as an undergrad during this time. I was responsible for bringing the clean plates out. I see this guy pick up the stack of plates to take the plate from the middle of the stack and I judge him. Thinking in my head, I'm like, “Why didn't the guy just take the plate on the top of the stack? What a weirdo?” I just keep walking on like, “Oh, hum.” Then all of a sudden, 20 seconds later, it hits me, I'm like, “Wait a second--“ A few months before that, not only did I never take the plate from the top of the stack, but that was the absolute least neurotic thing that I ever did around food. I was the one responsible for cleaning the dishes. Even I would spend 20 minutes picking out a glass that was clean enough to drink out of.
As I had told you before, quite often, I couldn't eat anything. Then it just hit me that I not only had my mental health undergone a complete revolution since I had started eating along the principles of Weston Price, but this change was so stark, and so dramatic, and so completely-- I was so mentally, completely different from how I'd been that I didn't even remember being like that just a few months before. The tiniest example of food neuroticism that was nowhere near as deranged as anything that I was engaged in at that time, even that just seemed completely foreign to me. That experience was incredibly profound. The tooth decay also stopped as a sidenote. That was the real thing that pushed me into my current career because I wanted some way to pay forward what I learned. I thought of going into medical school. I as well as my professors and the people that I worked with and friends, there were just many realizations from me and from others around me that I was much more suited to doing research than medicine. In particular, I think that with my analytical brain, I'm much better at cracking puzzles and coming up with solutions that other people can use to improve their health rather than taking a body of knowledge of what is known and applying it over and over again. I feel those are the big differences between what medicine would have been and research. And so, that took me to my PhD in Nutritional Sciences and into my current position of independently creating science education around that topic.
Melanie Avalon: Wow. Okay. I was hoping you were going to tell the plate story. So many questions just from that. I think my audience is going to be really excited to hear this conversation, because-- I bring on people from all different perspectives on the show and I think people get a little bit confused and overwhelmed, because one day, I'll bring on a carnivore person like Shawn Baker or Paul Saladino. Last week, it was Dr. Neal Barnard, who was very much in the vegan camp.
Chris Masterjohn: I had a debate with him once on Intelligence Squared.
Melanie Avalon: Oh, really? How did that go?
Chris Masterjohn: It was me and Joel Salatin against him and Gene Baur, the author of Farm Sanctuary. The motion was, don't eat anything with a face. We lost the debate based on a larger percentage of audience voting, either neutral or for our position, who shifted to their position at the end of the debate.
Melanie Avalon: It was wonderful to have him on the show. I was really surprised because I didn't reach out to him. His people actually reached out to me. It was hard to get answers. The biggest comments that I've been getting on that episode because it just aired is that he didn't really answer my questions, but that's okay. Going back to the plates, and the neuroticism, and all of that, so, one of the most controversial things I think I have aired on this show, a statement that was made by a guest that sparked a lot of controversy was, I had Dr. Natasha Campbell-McBride on the author of The GAPS Diet. She was talking about how people who are vegan often have these episodes that they don't even remember where they go and eat nonvegan foods. Have you heard of that happening?
Chris Masterjohn: I've never heard of that happening, but I will tell you two things that I know of. One is that if you look at survey data, the vast majority of people who report being vegan or vegetarian report--actually report occasionally eating chicken and fish. There's a very large percentage of people who identify that way and yet, even though they're identifying with something that's an absolute principle, they are in practice just generally eating that way, but not all the time. Then I will also tell you that I, in fact, have very patchy memory from when I was a vegan. Actually, my mother told me in the last year or two, I didn't remember this at all that during that time, I had gone to the emergency room during a panic attack like seven times.
Melanie Avalon: And you don't remember?
Chris Masterjohn: I remember one of them. [chuckles] I don't remember seven. Yeah, so, I don't think that I had times where I blacked out and ate chicken. But apparently, I had times where I blacked out and a lot of vegans eat chicken.
Melanie Avalon: So, it is a possibility. There's a study that is really interesting that they were looking at the brains of vegans. I don't know if they were comparing it to vegans. I think vegans and omnivores. When they looked at a piece of meat and basically, the conscious part of the vegan brain didn't light up. They didn't perceive that they wanted the meat, but the subconscious desire parts of the brain did light up. Paul Saladino talks about it. I thought it was really interesting. So, what do you think is happening with people? Because there are people, well, so they say, who are vegan lifelong and with longevity? Let's just throw out Loma Linda, shall we? What do you think is going on there? Is it possible?
Chris Masterjohn: Oh, sure. I have no reason to doubt that there are people, who do veganism long term and thrive on it. There's not a whole lot of them. We're dealing with a small anecdotal sample size. If you look at the data, just survey data generally indicates that x vegans outnumber current vegans by two to one. It would seem that with any given cross-sectional slice of time, there are more people by a factor of two to one or so who don't do well on a vegan diet than who do. Of course, I think you probably have some selection bias in favor of people who would do well on a vegan diet actually doing a vegan diet. I'm quite sure that if you randomly allocated people to a vegan diet that you just allowed people to follow how they felt. I'm sure you would wind up with way more than a two to one ratio having a negative experience with a vegan diet. You're selecting for the people that are good candidates for it and you're winding up with a two to one attrition rate. I think that generally speaking, people don't do well on a vegan diet, but that third of people who stay on it for some given amount of time and the anecdotes of people who do well on it and thrive on it, I have no reason to think that they're lying or deceiving themselves or us. That might be happening, but I would rather just simply acknowledge those stories and say, “My way to reconcile the good experiences or the bad experiences is to invoke the clearly true fact that people are very wildly in their nutritional requirements.”
If you look at a vegan diet, it generally can supply all of the essential nutrients as defined in a textbook, where it's particularly weak-- if it's well designed. Where it's particularly weak is on issues of how well absorbed are some of those nutrients from certain foods, some of those nutrients have to undergo metabolic conversions in order to be useful. The animal form of that nutrient might be different than the plant from that nutrient and the animal form of that nutrient is closer to what or is what humans require. Some people might be better at making that conversion, some people worse at making that conversion. And then of course, there are many things that are present. The animal foods that are not classified as essential nutrients, but still might be health promoting. The absorption of calcium from different foods is not just dependent on calcium would be one nutrient where it tends to be less well absorbed from plant foods than from animal foods or from many plant foods and animal foods. Not only does that depend on this particular food that you're eating, but it also depends on the person's gut. You're going to have variations from person to person on calcium absorption from the gut. The nutrients that require metabolic conversions examples include vitamin B6, vitamin A, essential fatty acids. Some people are great at making those conversions from plants and other people are terrible at it. And so, there's going to be a variation around that.
Then on things that are not classified as essential nutrients, but are found exclusively in animal foods whether it's carnitine, or carnosine, or you name it from animal foods. The plant and the animal foods are just full of all many thousands of things that are not essential nutrients might have some health value of consuming them. It's generally not well studied when some people worse than others at making something. Creatine, I guess, is an example. Different people's synthesis of creatine is different and this is something that you can get from animal foods. You can't get from plant foods. But no one really studies the synthesis of creatine. No one cares. Because there're very rare defects in creatine synthesis that are exceedingly rare. Those get studied, but they're not thought to have applicability in other people. But if it's not considered an essential nutrient, no one's really out there trying to study or there're some people that need this under some conditions. Just generally, our knowledge of those things aren't very good. But I would not be at all surprised if variations in the ability to synthesize things like creatine, carnitine, carnosine, and so on, or cholesterol even are contributing to why some people just do terrible on a vegan diet and others do fine.
I think it's totally plausible that there are certain people that because of their constitution, genetics, gut, etc., they don't have a problem eating a high-fiber diet, they don't have a problem with plant toxins, they don't have a high need for animal-based non-essential nutrients. They are great at making metabolic conversions from plants for vitamin A, for vitamin B6, or essential fatty acids. They are great at absorbing calcium from the gut, just all these factors that you could list. They just check the boxes on all of them, and so they're pretty compatible with a vegan diet, and those might be the people that thrive on it. But there're a lot of boxes to check. It might be quite rare in the population that someone checks all the boxes. And you really only have to not check one of the boxes to have a bad experience on a vegan diet because if you're terrible at converting the plant form of vitamin A to the form that you need, and you check all the other boxes, you're going to wind up with a vitamin A deficiency. It doesn't matter if you're great on all of your other nutrients. If you're deficient in one of them you're going to have serious problems. Yeah, so I see no reason to think that there's not some people who do great on a vegan diet.
Melanie Avalon: Okay, that touches on something that I did have a huge question talking about the potential to synthesize certain vitamins and our requirements. It explains based on what you're talking about earlier with Weston Price and realizing that all these different populations ate one of these four food groups. I'm very much curious how humans as species evolved with different societies and different ways. How can we have such similar needs? How can there be blanket statement dietary recommendations for the nutrients as a human regardless of your genetics, your ancestry? And then, so, I guess, the first question is, are these RDAs and I guess, you could talk about the official RDAs versus what the actual RDAs might be. But are the RDAs pretty consistent regardless of your genetics and your background-- your genetics and your background. And then two, that ability to synthesize or not, is that based completely on historically what you would have been exposed to or does it also affect the amount that you actually need? If you're not able to synthesize something as much does that at all mean that you don't need it as much or you still need it, it's just historically you didn't need that genetic pathway to synthesize it more?
Chris Masterjohn: Well, I'll answer the second question first. Generally, if you can't synthesize something you needed that is-- the evolutionary explanation for that would be you had it and so, therefore, you didn't need to synthesize it, which means that you needed more.
Melanie Avalon: If you can't synthesize it, you would need it even more in your diet, does it actually affect the total amount that you need compared to somebody else or is that pretty consistent?
Chris Masterjohn: Well, okay, let me go back to your first question before I answer that, because your first question was about amounts. The RDAs, so, there's the National Academy of Medicine, which used to be until recently was the Institute of Medicine. Their food and nutrition board sets the dietary reference intakes are DRIs. Within the DRIs, there are minimal amounts, and upper limits, and various other values that feed into them. The most popular of those is or the one that people pay the most attention to is the RDA, which is the recommended dietary allowance. And then when there's not enough evidence to make an RDA, there is an AI or an adequate intake. And then there also are tolerable upper intake levels, which usually people, if they refer to them at all, just call them the upper limit, those are set for some nutrients and not others just based on whether there's any known toxicity. And then very recently, just with the salt and potassium guidelines, they came out with a new one, which is, I don't know if I remember it right. I think it's the chronic. It's something like the chronic disease reduction requirement. I'm messing it up. But it's one that's aimed at not preventing a deficiency disease, but rather reducing the risk of a chronic disease.
Then when people look at the values on a food package, usually, those are the daily values that are set by the FDA. They are not set by the National Academy of Medicine and they are not part of the group of DRIs that I was just talking about. But they usually are derived in some way from the DRI said by the National Academy of Medicine. But actually, there are some very significant discrepancies. For the longest time they were recently revised, but for most of our lives, the daily values are actually using old DRIs from significantly longer ago. And so, you would see, for example, that the daily value for biotin was 10 times higher according to the FDA than the adequate intake set by the Institute of Medicine. There are definite discrepancies with what you'll find on a food label for these. But dietitians will usually utilize the DRIs, food tracking apps will often, they may be using the daily values or the DRIs you would have to look. And then if you google what's the RDA for something or what's the upper limit for something, you're generally going to find the DRIs.
Okay, so, the RDA, when there's an RDA set for a nutrient is set on the assumption that the amounts-- This is where I'm getting to the answer to your question about variation. The RDA assumes that there's variation in the amount that different people need of a nutrient. The RDA is not meant to be used by an individual to say you need to consume this amount. Rather, the RDA is basically set for a population. First, what they do is they calculate an estimated average requirement or EAR for a population. And then they try to make the RDA cover 97.5% of the needs of that population. Usually, this involves assumptions rather than data. That's because usually they have no idea what the variation and the need for a nutrient in the population is. The standard thing that they do is they say, “We have no idea what the variation in the need for this nutrient is. So, we will assume that it is normally distributed, which means that it takes the shape of an ideal bell curve. And we will assume that, so if you have data that that takes the shape of an ideal bell curve, two standard deviations covers--” If you take the mean and you go up two standard deviations, you'll arrive at the 97.5% coverage point. You have 2.5% of the area that bell curve is left out. They assume that there's a bell curve of some variation. They say, “We have no idea what that variation is, but we'll assume that a standard deviation is 10%. And so, we will cover the need for 97.5% of the population by taking the estimated average requirement and multiplying it by 1.2.” In other words, adding the two standard deviations of 10%. So, adding 20% to it to cover the needs of 97.5% of the people.
Now, one of the problems with this approach is that anytime they ever do have any data on the variation in the need for this nutrient, it's way higher than 10%. There's never been a nutrient where they've measured the variation and the needs for the nutrient in the population and arrived at something as small as 10%. But for very long time when the DRIs were being set, the person who was the chair of the committee over, actually, probably the majority of the DRIs that are set was at that time very concerned that if you set the RDAs too high, everyone would go out and be supplementing, then we'd wind up with a mass vitamin toxicity problem. Under this concern, they systematically erred on the side of setting the DRIs to be in the absence of knowing exactly where they should be on the lower end of where they thought they might turn out. If you look for example at niacin, niacin is a case where they had four studies that all estimated the variation in the need for niacin. Those studies were suggesting that the variation was more 30% or 40% was the standard deviation. If you look at the paper that they wrote in justifying the DRI for niacin, they said, “Clearly from these studies, the variation in the need is greater than the customary 10%.”
They're saying this on the basis of a finding that it's 30%, 40%, 45%. They say, “Given that it's clearly greater than the customary 10%, we don't know exactly what it is. We're going to say it's 15%.” The RDA for niacin is set on the estimated average requirement multiplied by two standard deviations of 15%. In other words, multiplied by 1.3. That's how they get the RDA. But notice that the actual measured variation was still more than twice what they said it was. The two things to take away from this are that the whole idea of the RDA assumes that there's variation in the population not that everyone needs the same thing. The RDAs is not a blanket recommendation for everyone to eat the RDA. That's not what the RDA means. The RDA means that if you eat that amount, you basically have a 97.5% probability of meeting your need for it. But the RDAs systematically underestimate the variation. And so, what you would expect from that is that many, many people are getting their needs filled when they're eating the RDA, but some percentage of people that is larger than the expected two and a half percent are not getting their needs met.
Melanie Avalon: If we follow the RDAs, we have a 97.5% chance of getting enough based on the range of what they're going on for what people might actually need. But it might actually be much a much larger range than that.
Chris Masterjohn: Yeah. That's putting aside all the other questions about how has the science evolved since the RDA was made and was their analysis of the science at that time good? Just on a purely mathematical basis, if you eat the RDA, you have a 97.5% chance of getting enough for your needs. If you assume that their assumption about the variation is as small as they assumed it to be, but all the evidence indicates that it's not, and so, I don't know what the percentage is. It's not getting what they need when they eat the RDA. But just on mathematical grounds, it has to be larger than that 2.5% that they say it is. Most people don't know that the RDA is designed to give you a 2.5% chance of not getting enough of the nutrient, though.
Melanie Avalon: That is a mind-blowing fact for today. Never look at the RDA the same way again.
Chris Masterjohn: Oh, wait. Can I give you one extra fact about that?
Melanie Avalon: Please do. I love extra facts.
Chris Masterjohn: Because I find this an infuriating scam. Going on this concern that we don't want to tell people that the whole population is deficient in something or we're going to create-- Well, I think on the DL, they're concerned that they will make themselves look bad if they're the nutrition experts that are managing the population. They published data about how the populations intake of nutrients sucks, because they're in charge of the food supply and they want to say-- It's like when they publish data about what the population is taking in, yes, they want to identify problems and fix it. But it's like a State of the Union address. You don't want to come up and say, if you're the president you don’t come out and say, “Well, the State of the Union sucks.”
Anyway, the guidance for using the DRIs to measure population level intakes is to say that you should not use the RDA as a metric. You should use the estimated average requirement of a metric. What they say is, “If you're measuring the average intake in the population and you want to compare it to something to see if it's good or not, you should use the estimated average requirement.” Because if the average intake is as good or better than the estimated average requirement, then everything's great. But this is based on a preposterous premise, which is that if the intake of something varies in the population, that it is automatically varying such that the people with a high need for something are eating more of it and the people with a low need for something are eating less of it. Yes, there's variation around the average. But actually, there's literally nothing stopping the people who need the highest intake of vitamin A from eating the lowest and the people with the lowest need for it eating the highest. If the average intake is meeting the average requirement, that's equally consistent with everyone getting enough and everyone being deficient.
Melanie Avalon: It could go either way. Yeah.
Chris Masterjohn: Right. Yeah. And presumably, it's random. Presumably, there also is no reason why the people with the highest need would eat the lowest intake. So, that's—[crosstalk]
Melanie Avalon: Well, people's cravings naturally drive them towards going what they need?
Chris Masterjohn: Generally, not. You could hypothesize that, and it's a reasonable hypothesis, and it's worthy of research. But generally, the science indicates that rats are more likely to do that than humans. Just look at how people eat. People obviously crave hyper palatable foods that make them fat and don't crave things [laughs] are health promoting. When was the last time you saw someone who is craving liver versus ice cream?
Melanie Avalon: I have a question about that actually. Sorry, not to go on a rabbit hole.
Chris Masterjohn: Okay. Well, let me just finish the statistical point and then we can go straight to that question. The point is it's equally unlikely that the people are going to be eating opposite to their needs as they are going to eat beating perfectly to their needs. Absent specific evidence of it, the assumption should be that the variation around the average intake is driven by random factors that are at least random to with respect to the unknown physiologically driven needs of someone. I believe that when you're looking at the population and you're trying to identify the nutrients of concern as they call them, you actually want the population to on average be eating somewhere around the RDA. Because if the RDA covers 97.5% of the needs of people, then you don't need to know their needs. You just know that if that's true, if the RDA principle is true, then 97.5% of people are meeting their needs, the average person is eating the average intake, then all that tells you is the person in the middle, who's eating the middle of--
Actually, it doesn't even tell you that. It basically doesn't tell you anything about whether the people are meeting their own needs. I just find that infuriating statistical error, but I don't think it's quite an oversight. I think it's driven by them not wanting to say that the population is by and large eating a diet that's not very nutritious and an irrational fear that will get people over supplementing into the toxicity range if we revealed to them that they might be shy on their nutrients. So, it's a massive cover up of the state of nutritional adequacy. But anyway, I'm done with that rant.
Melanie Avalon: So, the way to be most transparent, I guess, is not practical, which would be to for every nutrient say, this is the range from here to here and we don't know what you need in that range. What's the practical solution?
Chris Masterjohn: That would be the most transparent thing to say, although, I think you have a big problem trying to translate that onto food packages.
Melanie Avalon: Yeah. [unintelligible [00:43:48] so well. That idea that they have this fear of people having supplement toxicity, what do you think is more dangerous, erring on the side of deficiencies or erring on the side of over supplementation?
Chris Masterjohn: I think that overwhelmingly with nutrients, you have a huge window, where you can get more than you need without getting toxic. These aren't pharmaceutical drugs where the risk profile is such that there's no principled assumption of safety through any exposure range. Generally speaking, humans have overconsumed-- One of the points that Weston Price made was that, “If you measured the nutrients of these extremely healthy people on their traditional diets who had not gone through modern industrialization, they generally like fourfold overconsumed their basal requirement.” His point was that if the diet generally fourfold overconsumed the nutrient, then as you go through life and you encounter numerous things that raise your requirement above the basal requirement, you don't run deficient. If you get pregnant, yeah, there're special diets for pregnant women that will overconsume pregnancy related nutrition even a little bit more than that. But if you randomly get pregnant when you weren't specifically preparing for it, you are coming from a background where you know you're not deficient. If you don't know that you're pregnant, you are automatically consuming enough for pregnancy by default before you figure it out.
If you get injured and now you have to heal, all these different things that might raise—Or, as a child, if you're growing, all these different things that could raise your requirements for the nutrients, the default of the diet is just set, so that you are hitting on the higher side of where your needs might go rather than getting the bare minimum. If you're trying to target the minimum all the time, then all it takes is the slightest rise above the basal requirement. The slightest injury, the slightest illness that you have to heal from or fight off, or the slightest wound to push your requirements slightly above that, so you're running a marginal deficit. Why would you want to be flirting with a marginal deficit all the time? It doesn't make any sense. But getting back to another point, that's a little bit closer to what I think the way you were asking it. Because that's been our ancestral strategy, it's really clear that we can overconsume our needs by a factor of three or four and not result in toxicity. But it's also just true for modern science.
If you just look at where the Institute of Medicine set the upper intake levels relative to the RDAs, they were almost always several fold or way more than that above the basic requirement. For example, let's take a random one. The RDA for vitamin B6 is less than two milligrams a day and the upper limit is 100 milligrams a day. Yeah, you can have debates about should they lower the upper limit or whatever? But my point is that this strongly implies a very huge window where if you're consuming three, or four, or five milligrams, you are way above the RDA, but you're nowhere near the upper limit. I think it's just very clear on the principle of having a large window between the minimal requirement and the toxicity, this has to be the case that you would want to be nowhere near either end of that window. Being 20% into that window might take you three or four times above the minimal requirement for the nutrient. But if you're nowhere near toxicity, why wouldn't you want to be there? Why would you want to be anywhere near flirting with the edge of deficiency?
Melanie Avalon: That range for toxicity, does it range or is it pretty set in stone? Is it the same as the deficiency?
Chris Masterjohn: Oh, well, it's probably the same in principle, but the data is always very sparse. They don't set it like that. The way that they set it is they look for a no adverse effect observed level and a lowest adverse effect observed level. They try to impute where the true value of the lowest observed adverse effect and then they multiply it by an uncertainty factor. And that uncertainty factor because you're trying to protect against toxicity brings the upper limit lower than where it would be without that uncertainty factor. The poor the data is, the more conservative you are. And so, for vitamin B6 in the example I just gave, the evidence was very poor about where toxicity started. The lowest dose used in case reports of neurological disorders that could be caused by it, were using 500 milligrams of vitamin B6 per day. They said, “Because the data is so sparse and so unclear, we are going to use a safety factor of five.” They divided 500 milligrams by five to get 100 milligrams.
Whereas in other cases where they know a real lot about that data, they'll use a very narrow uncertainty factor and they might decrease the upper limit by 30% or something like that because of it. There obviously is going to be people that do not get a toxic response above the upper limit. But they don't try to characterize what that distribution is. The RDA is designed so that 97.5% of people will get enough getting it. The tolerable upper intake level is placed outside of the curve on the left, so that there's some bell curve of toxic responses across doses above the tolerable upper intake level, but you're not trying to be part of that curve at all. You are trying to be way to the left of that curve, meaning, a much lower dose of the nutrients, so that you're not even in the curve. The distribution theoretically exists, but they're not trying to characterize it because they're just trying to not be part of it. They're saying, “There's some bell curve of distribution over there,” but we don't care what it is. We're going to stay over here. We're going to go nowhere near that bell curve.
Melanie Avalon: The question that I thought of when you're talking earlier that you touched on, this is something that has haunted me for so long and it has to do with cravings of things. You talked about people don't go out craving liver. Liver is one of those “super foods.” It has all of these different nutrients in it and it's often prescribed as a food to turn to for nutritional status. But I feel there are so few people that naturally like liver. It's hard to get people to eat liver. Even people following a Whole Foods based diet, even I, I pretty much love everything, but plain liver, I just can't stomach. Why is that? Why do we not have a craving for liver? I don't want to make a blanket statement, but I have noticed this just in general when it has so many nutrients, is it because of toxicity issues?
Chris Masterjohn: That's plausible and worthy of investigation, but I doubt it. I don't know if you've ever talked to Stephan Guyenet, but I think you would be a great person to ask about this as well, just on the topic of-- he's a neuroscientist, too. We look at a lot the same stuff, but he comes from more of a neuroscience background. But my answer to that would be, first of all, rats do crave liver. If you go way back in time back to when they used to feed rats actual food, now, lab rats are typically getting purified diets that have each component put together into a pellet.
Melanie Avalon: Yeah. Which I feel messes up, I don't know, a lot of potential findings.
Chris Masterjohn: Well, it depends on your perspective. What really messes up a lot of potential findings is the fact that they don't give rats toys, so that they don't move. Because if you try to make rats fat, but you give them a hamster wheel, there's no way you can make them fat. You can't feed them anything that makes them fat. Sidenote, when I was in grad school, while I was talking with my advisor about toys, because the veterinarians were-- If you were on animal experiments, your animals are in this high security place, where they have vets on call 24/7. There's staff that take care of the animal place and you just go down there to feed them. Well, part of the security is to not get pathogens and part of the security is to not get blown up by animal rights activists or something. When I did my postdoc, the animal facilities were not placed on the maps of the school and they were like these doors that you wouldn't notice to get there and you had to get your scannable ID had to get modified, so, you would have permission to get in there, and there's this door that leads to this white hallway to this other door. It's very hidden. But also, you have to go through this protocol to enter this transition room, where you put the clothes on that are going to stop you from tracking in any pathogens or whatever. But anyway, that's not the point.
The point is, the veterinarians were always very pro toy. They always felt that the animal should be given toys, because it's good for their mental health. I was talking to my advisor about this and he was always very anti-toy. The conversation was basically like, “Well, look, if you give them toys, you can't give them dietary-induced obesity. You can't study anything about dietary-induced obesity.” We studied fatty liver disease and one of the models was in dietary-induced obesity, because if you induce obesity with diet then you will also induce fatty liver. Because if you make an animal fat, you make their livers fat as well. Then that would allow us to study other things just for their protective effect against fatty liver disease. He's like, “If you give them a toy, they're not going to get fat. If they don't get fat, then they don’t get fatty liver, if they're not going to get fatty liver, how you're going to study green teas impact on fatty liver disease?” I said, “Well, wouldn't it be more realistic if they were given toys because then you would have a more realistic view of what actually induces obesity in them?” He said, “We're not about natural, we're about control.”
What he meant was, it's not about trying to reproduce a realistic environment. We're about trying to create a reliable model of a disease, so we can study the disease. As long as you control the fact that none of the animals get the toys, then that's a good model. Whatever you did change your experimental variable, you know that's the only change in the animals that got that variable that you want to study. Well, look, there's a problem of generalizing from animals to humans no matter what. There is another problem if it's not realistic for the life of an animal. But it's also you're already so removed from real life anyway, the real life of a rat, just by the fact that you have all these inbred or otherwise highly controlled breeding of rats and mice, these animals are already bred to be specific models of disease and not the subway rat or the wild ground rat. And so, yeah, you are removing them from reality another step by using a purified diet, but the reason they made those diets in the first place was because they wanted to be able to study the toxicity of a toxin or the carcinogenicity of a carcinogen, and they didn't want all these random things getting in the way like you blended together a bunch of food, but in that batch the food was high in selenium and in that batch it wasn't. So, that's why they evolved that way. So, it's a tradeoff. You have more highly controlled experiments, but you can question how relevant they are, even the animals that are eating whole foods. But then again, even if they were eating whole foods, you really have to be careful about generalizing from a rat or a mouse to a human anyway. It's not making or breaking the science really, but it is important to acknowledge that.
Anyway, back in the day, when they used to feed animals foods, they did experiments where they just looked at the preferences of the lab rat for different foods. What that generally showed was depending on what other food was available, they tended to eat, they tended to choose foods that fulfilled their nutritional requirement. For example, they would always highly prioritize liver. But once they ate a certain amount of liver, they'd stop eating it. They wouldn't overeat the liver. They craved the right amount of liver. If you gave them a lot of white flour, they would specifically choose out wheat germ in the ratio that would balance the original flour, the original whole wheat flour. But if you gave them just wheat germ and you didn't give them white flour or you gave them wheat germ and whole wheat, they would eat the whole wheat because it was already balanced. They would only eat a lot of wheat germ if they also had white flour to balance it, to try to reconstruct the whole grain. Those experiments suggest that there is something in animal life that at least exists in rats, that it's very much geared towards trying to choose out the foods that are good for us.
Now, in humans, I don't know. If you look at the work of Weston Price, he clearly identified traditions around eating foods that they knew were needed to nourish them. But if you look at the body of knowledge they had, two things arise. One was, Price was very emphatic that strength of character to go out of their way and get these foods was very important. He made it sound very effortful that they were going out to get these foods. He didn't describe populations that were just like, “Oh, we love liver and we are lucky because of it.” It was like, “We're going to go out of our way to prize these things and to develop a culture around eating them, because we know that they're good for you.” But also, if you look at what they knew about why they were good for you, they're things like we know that you can eat eyeballs to cure blindness. And so, what kind of blindness is cured by eating eyeballs? Vitamin A deficiency blindness. The Canadian natives of the Arctic, they knew that they could cure scurvy with eating adrenal glands. When the moose were in mating season, they would cut out what they call the little ball of fat above the kidney, which was not a little ball of fat, it was the adrenal gland. They would cut up it into pieces and they would give every little Indian and every big Indian in the tribe a piece of adrenal gland, and that's why they didn't get scurvy and why scurvy was a white man's disease.
But the fact that they knew that indicates that they did get scurvy. How would they know how to prevent scurvy with adrenal glands if they didn't get scurvy? That is particularly consistent with the fact that humans needed more than their cravings to eat a good diet. They needed a body of knowledge that was passed down over generations where they clearly had experience with nutritional deficiencies. Now, that doesn't mean that they got nutritional deficiencies, because they had completely lost the cravings that other animals have for nutritious foods. It's quite possible that just limitations in their environment, it could have been that they knew about these deficiencies because of access issues. For example, in a new environment where the foods were different, or in a disaster, or a case of overhunting, or in marginal environments like in the Arctic, it's very hard to get certain foods during certain parts of the year. All of those could have created opportunities for deficiencies that then layered on top of their natural cravings for good foods, a body of knowledge that would make them more robust to those deficiencies. So, that's plausible, but then you have to ask, “Why, you don't know anyone that loves liver?” Well, I was interviewed by a guy who lives in-- I think he lives in the city now, but he's from a Greek village and he said that people fight over the organ meats. During Lent, they’ll fast from animal products and then on Pascha or Easter, they will eat lamb, but they fight over who gets the brains, and who gets the liver, and stuff like that.
I think it's possible that these are-- I could come up with two hypotheses. One is that these are totally cultural. If you have the body of knowledge that liver is so important, you teach your kids that from a young age. During development, because the liver and their body feels how they respond to it and because that's also reinforced culturally, they develop a craving for it, because they have programmed their response that way during development. Then later during adulthood, they still have that programmed response. So, that's one hypothesis and these aren't mutually exclusive, but another hypothesis would be our reward system in our brain, in our society, it has been completely demolished and deranged by eating hyper palatable foods. It might be that that system actually works normally by default if you don't throw at it, foods that have been designed to manipulate it. It just gets completely deranged through development being constantly barraged with foods that are designed to manipulate it, make you eat more of those bad foods. And also, a culture that reinforces that. Our culture doesn't know anything about the value of organ meats and very much treats junk food as a thing to aspire to.
Yeah, there's health culture that demonizes it but I think most of us when we grew up, grew up with cultural reinforcement of like, “Oh, I ate a good dinner. Now, I get to eat ice cream.” These things were like cultural rewards as well. I don't know. I guess, the interesting question would be like, if you-- The thing is, you can't raise a human with no culture. As a thought experiment, it's interesting to think about like, “What if you raised new humans in a completely free choice environment and taught them nothing about food? Would they have a craving for liver?” I don't know.
Melanie Avalon: There was a woman who studied this. I was reading about it in a book recently and she had kid like-- baby or I don't know how old they were. They were really young. But they were given free access to a range of foods and it included foods like this. The breadth of the foods would cover their “nutritional requirements” and then went to see what the kids would do. They did naturally eat certain foods. It was like what you were saying before, where they were like the rats eating the liver, and then when they get enough, they're done. It was very much that effect and it was a lot of like weird foods. I'll find it and email it to you.
Chris Masterjohn: That's interesting and it makes me wonder how that would evolve over time, because I guess, what I'm wondering is, what is causing the disconnect? Is it more the absence of those foods, so, they can't be wired up with brain preferences during development or is it more that other things are just obstructing this? Are those babies? Are they learning in real time that when they eat a certain food it does something physiologically and their brain makes a new connection and identifies that as a source of nutrition or do they come preprogrammed with an instinct that then would stay as long as if it's not completely overridden by other foods designed to hijack that instinct? I don't know.
Melanie Avalon: Yeah. Speaking to that, so, the second hypothesis that we're clouded by these hyper palatable foods, my experience-- I think that's probably happening with a lot of people. But then my experience, I've been eating a very Whole Foods diet for a long time. I found that once I cleared my diet of the hyper palatable foods that I started naturally craving Whole Foods. But I went through a period where I was severely anemic. By the way, I love all of your work on iron metabolism and all of that. But in any case, at that moment, I was like, “If there's a time that I would love liver, it should be now.” So, I went, and I bought some liver, and I was like, “I'm going to like this because I like Whole Foods now, I like meat, I'm very anemic. I'm going to like this” and I didn't. I had a lot of cognitive dissonance surrounding that. I don't know if it's like-- I don't know. [chuckles] It was an interesting experience, though.
Chris Masterjohn: To be honest, the only people I know that like liver or people that grew up eating it. I'm very immersed in the population of people that eat liver. [crosstalk] I've spent almost 20 years in the Weston A. Price community and liver’s a big deal in the Weston A. Price community. When it comes down to it, if I talk to people in or out of that community, everyone there eats liver in some form. Some people take capsules or—[crosstalk]
Melanie Avalon: I grew up eating it. My grandmother was German. It was that salty in the past. I don't know. It's all mixed up. It's like the pate. I don't know. No, it's not pate. It didn't taste like liver. Just getting a hunk of liver plain.
Chris Masterjohn: Yeah. Well, I don't like liver. I feel better when I eat it. My favorite way to eat it is with a blend of other organ meats and ground beef with a lot of tacos seasoning as crumbles.
Melanie Avalon: Mm. Nice. Can't taste it. [laughs] Okay, you’ve touched on something else that I have massive questions about. I'm so excited that you brought it up. You're talking about the rats at the labs that you would study when you're a grad student. I heard you on Peter Attia talking about your work with that, and what you found about choline and fatty liver. I've been obsessed recently with fatty liver, because I recently interviewed Dr. Rick Johnson for his book and then David Perlmutter has a book coming out on uric acid. I've just been awash thinking about fatty liver, and fructose, and all of that. I was wondering if you could talk a little bit about choline and how it may affect fatty liver. I actually told Rick Johnson that I was interviewing you and he is dying to hear more information about this. He was not familiar with these studies.
Chris Masterjohn: A fatty liver disease is an accumulation of fat in the liver. The amount of fat that accumulates in the liver can basically be summarized by the equation, fat in minus fat out. As long as under fat out, you also include fat that is burned for energy in the liver. You could separate those. You could say, it's fat in minus fat out minus fat burned. It would be one way to put that. Anything that can lead to fat going through the liver will increase the risk of fatty liver, anything that brings fat out of the liver will decrease that risk. If you look at just generally who gets fatty liver, it's very closely tied to obesity.
The reason that it's closely tied to obesity is that when you are overweight or obese, so, actually, even if you're lean, you constantly have fat being released as fatty acids and glycerol that goes to the liver, and gets turned back into triglycerides, and leaves the liver as triglycerides. That cycle is operating in everyone all the time. And so, even if you're not eating any food this is going on all the time. Just by having adipose tissue, your liver is exposed to a source of fat in. If you have more visceral abdominal fat, then that in particular will be way more risky because the visceral abdominal fat pad empties directly into the liver. Every other fat in your body empties into the bloodstream. If you're emptying fat out into the bloodstream, then some of it becomes part of the fat inequation for the liver. But if you have a visceral abdominal fat and everyone has visceral abdominal fa, some people have more than others, then all of the fat released from it becomes fat in in the liver.
Now, generally speaking, when people are obese, they have way more visceral abdominal fat than people who are not obese. There will be variation. Someone who's obese and has a higher fraction of their fat has visceral abdominal fat will be more at risk for fatty liver than somebody who's obese and has more subcutaneous fat. But just being obese raises-- All adipose tissue contributes to this risk to some degree and the visceral abdominal portion is the major risk. But generally, certainly, for any given individual, if they get fat or leaner, they're directly increasing their visceral abdominal fat or decreasing it. Now, eating fat increases the amount of fat that goes into the liver and eating fructose can increase the amount of fat in the liver because fructose compared to starch is more lipogenic. Meaning, it's more likely to be converted into fat in the liver than starches. If you rank macronutrients by how much fat they'll put in the liver, the fatty liver contribution potential is highest with fat and its lowest with starch. Now, protein is a whole another animal, and I'll get to that in a minute, and it highly relates to the choline story. Among fats, the ones that are more easily burned are the least likely to contribute to fatty liver. Generally, chain length and saturation all increase fatty liver potential. MCT oil, which is shorter chain is less likely to contribute to fatty liver than olive oil, which is long chain fat. But all things being equal if you're eating more saturated fat, tallow versus olive oil, the tallow is going to contribute more to the fatty liver.
Now, actually I should clarify. When I say contribute to fatty liver, I just mean contribute to the fat in portion of that equation. That doesn't mean you could eat a 100% tallow diet and not get-- Well, not a 100%. But you could eat inordinate amounts of tallow and as long as you're fat out part of the equation or fat being burned part of the equation is operating to match it, you will never get fatty liver disease. Okay, so, what experiments early-- And of course, alcohol is also lipogenic and also harms the ability of fat to get out of the liver. For the longest time, alcohol was thought to be the exclusive cause of fatty liver disease. It started in the 1950s. There was research showing otherwise, but really in 1980s, it became acknowledged to the point where they started separating people who had alcoholic and nonalcoholic fatty liver disease. And that was partly because if people showed up with fatty liver disease and their doctor told them to decrease their alcohol intake, and the patient said, “I don't drink alcohol.” The doctor would say, “You're lying, your liver results show it and they would get sued.” [chuckles] They not wanting to keep getting sued or keep getting other types of complaints. They coined the term “nonalcoholic steatohepatitis” or NASH in the early 1980s. And then eventually, NASH became a subset of NAFLD or nonalcoholic fatty liver disease. NASH refers to the more advanced inflammatory stages, whereas NAFLD, nonalcoholic fatty liver disease is a broad umbrella that also includes simple steatosis, which just means you have more fat in your liver than you should, but nothing bad is happening to it yet.
Anyway, if you go back to the 40s and 50s in that era, even before they acknowledged this in humans, they already knew that you could give an animal fatty liver disease with sugar. Even before that, way before that, they knew you could give an animal fatty liver disease with fat. Actually, very early on, the first thing that they knew is that if you fed lab animals fat, the more fat that you gave them, the more they would develop fatty liver disease. But the more protein you gave them, then the less fatty liver disease that you would get. In fact, you could feed them as much fat as you wanted as long as you gave them enough protein to match it. It was early on known that there was some interaction between fat and protein. Later, they showed that no matter whether you gave an animal fatty liver disease with sugar, alcohol, or fat, as long as you gave them enough protein, they would not get fatty liver disease. They said, “Hmm, what is it about this protein?” They said, “Well, maybe it's the sulfur amino acids.” Then they showed that whether you give the animal fatty liver disease with sugar, alcohol, or fat, you can just give them the sulfur amino acids, which are methionine and cysteine, two of the 20 amino acids that make up proteins and they won't get fatty liver disease. Then they said, “What might these be doing?”
Their hypothesis was phosphatidylcholine, which is a form of choline that is a phospholipid that makes up cellular membranes is known to be needed to export triglycerides from the liver. They said, “Maybe what's happening is the sulfur amino acids are helping the synthesis of phosphatidylcholine,” because we know that they do that. They just gave choline and they found that choline abolished fatty liver, whether it was induced by sugar, alcohol, or fat. Collectively, what these experiments are showing is that sugar, alcohol, and fat can all cause fatty liver disease, but as long as you get enough protein, sulfur amino acids or choline, you don't get fatty liver disease. That's because protein supply sulfur amino acids, sulfur amino acids help you synthesize choline, choline you can synthesize using sulfur amino acids or you can just eat it. Then as long as you get enough choline in the liver, you increase the fat out part of the equation that it doesn't matter how much fat you put in, so, you could be fat, you can have high visceral abdominal fat, you could eat a lot of fat, you can eat a lot of sugar, you drink a lot of alcohol. As long as you're exporting that fat from the liver, you don't get fatty liver. And so, anything that helps you make choline being protein or sulfur amino acids is increasing the fat out portion of that equation.
Melanie Avalon: Okay, gotcha. Is that choline production demand driven or supply driven? If I eat a ton of protein will I just create excess amounts of choline or does it only create enough choline that it needs for that process or does it even matter? I eat so much protein. So, I'm very fascinated by this.
Chris Masterjohn: It's going to be, I don't know, if I want to say its demand driven, because you can't really make it happen without the supply. But the synthesis of phosphatidylcholine is actually, relatively constant as long as you eat enough to make it happen. I guess, the answer to your question is, as long as the supply is there, its demand driven and you can't really over produce it to stock up on it.
Melanie Avalon: Have they done studies giving high dose choline to rodents or whoever they're studying in a very lipogenic for fatty liver diet situation and absorbed it?
Chris Masterjohn: Yeah, that's exactly what they did in those early experiments. They created fatty liver disease through every means that they knew how and they showed that as long as they provided enough protein, sulfur amino acids, or choline then whatever they would do that would create that fatty liver disease wouldn't.
Melanie Avalon: Yeah. That's what you're saying when I was listening to your interview that the rodents that you guys used, you fed them casein or you did not feed them casein?
Chris Masterjohn: I fed rats 60% fructose diets and I expected it to cause fatty liver disease and it didn't. In retrospect, I believe that was probably because we used biotin supplemented egg white as our protein rather than casein, which is what is normally used. The reason that we did that was because our department head was very convinced that casein is inflammatory to rats and he was just broadly against feeding rats casein at all. We just routinely never used casein in the diets. He also thought that casein caused copper deficiency. For those reasons, we just never used casein in the diets. All the studies showing fructose causes fatty liver, liver uses casein in the diets and the egg white protein is way higher in sulfur amino acids than the casein is. In fact, casein is so low in sulfur amino acids that it's usually supplemented with methionine in normal lab rat diets but even the methionine supplemented casein is way lower in sulfur amino acids and straight up egg white.
Melanie Avalon: That is fascinating. While we're existing in the world of the different fats, and the saturated fats, and the chain links, I've read a lot of what you've written about polyunsaturated fats. There's so much debate out there surrounding PUFAs. First of all, you write about how the common, I think most people when they think EFA deficiency, they think omega-3s. But correct me if I'm wrong. Is it actually omega-6 deficiency that is more common or more likely to be an issue?
Chris Masterjohn: You mean an essential fatty acid deficiency?
Melanie Avalon: Yes.
Chris Masterjohn: Essential fatty acid deficiency is classically defined as a deficiency of omega-6 fatty acids.
Melanie Avalon: Most people think, I think omega-3s. Maybe that's just like a misconception out there.
Chris Masterjohn: Yeah. No, most people don't know anything about the history of it. Certainly, attention is much more on omega-3s since the 90s due to the interest in anti-inflammatory effects of omega-3s.
Melanie Avalon: How do you feel about--? I feel people are all on different sides about this. How do you feel about supplementing with things like fish oil, for example or more purified omega-3s?
Chris Masterjohn: I think it would be better to eat fish, but I'm not totally against using low doses of it in the area of hundreds of milligrams per day of EPA and DHA, if one doesn't eat fish.
Melanie Avalon: Okay, gotcha. Question, you talk about how DHA versus EPA and their role in addressing, or resolving, or preventing inflammation, and what is their role there and why is it that E--? Is it EPA that only can resolve inflammation if it's with aspirin?
Chris Masterjohn: Yeah. this also gets to the heart of some of the misunderstanding around omega-6s being inflammatory. If you peel back the last 20 years of research-- If you go back to the 90s and probably the 2000s as well, basically, everyone thought that inflammation was an active thing and that inflammation went away as a passive phenomenon. If you are inflamed because you're sick, the inflammation goes away later because you're not sick anymore. If you're inflamed because you got injured, like, the inflammation just went away after you'd healed enough from it. That was the idea that it's an active process to create inflammation, inflammation just fizzles out. As long as you remove the cause of the inflammation, the inflammation will go away or if you obstruct the creation of the inflammation, then you will stop it from ever happening in the first place. This is the basis of using anti-inflammatory drugs, especially the most popular drugs in the world, the NSAIDs or nonsteroidal anti-inflammatory drugs, the common anti-inflammatories you get at the drugstore. Acetaminophen is the one that's not an NSAID, although it basically does the same thing that the NSAIDs do. I'll get to that in a second. You could infer from that, that if anyone has inflammation, the problem is the cause of it. In other words, if someone just has chronic inflammation, it must be cut because of the chronic presence of a cause of inflammation. This whole framework is wrong. It's still the dominant framework in everywhere. It's still the completely dominant framework in pharmaceuticals, it's still the completely dominant framework in nutrition. Everyone still believes this.
You only believe otherwise if you delve into the literature on this topic. What that literature shows over the last decade or two is that the resolution of inflammation is not at all a passive process. It's a highly active process. If you can remove the cause of inflammation, but if you don't have the active process of resolving it, it will stay there forever. The fact that someone has chronic inflammation does not at all tell you that they necessarily have an enduring cause of the inflammation. It is entirely possible that the cause is long gone and they just aren't resolving it. Literally, everything that you could infer from the former framework turns out to be wrong in the present framework. Actually, it's worse than that because all of the anti-inflammatory drugs are based on either preventing the initiation of inflammation or somehow blocking its results. Ones that that people take the most are the NSAIDs and they are-- This is where I was getting at before like this is basically true of acetaminophen which is not one. All these common anti-inflammatories over-the-counter drugs-- Actually, this is also true of a lot of nutritional anti-inflammatories as well are reducing the expression or blocking the activity of the cyclooxygenase, or COX enzyme, which converts the omega-6 fatty acid, arachidonic acid into prostaglandins, such as prostaglandin E2, which initiates inflammation. This core complete misunderstanding gets at the heart of omega-3s and omega-6s, and it gets at the heart of NSAIDs, and it gets at the heart of what's the real cause of chronic low-grade inflammation.
The problem is not only that inflammation is an active process that you need to nourish, but inflammation-- I don't know if I said that right. Inflammation resolution is an active process you need to nourish. The real problem with pharmaceutically modifying this is that prostaglandin E2 made, and it's not just with pharmaceuticals, this is also a problem for trying to reduce omega-6s and increase omega-3s to address this as well. The problem is that prostaglandin E2, which is made from the omega-6 fatty acid, arachidonic acid, not only is the central initiator of inflammation, it is also the central initiator of the resolution of inflammation. If you're trying to bio-hack this, you want to believe that there's one chemical that initiates inflammation and a different one that initiates the resolution of inflammation. Because then you can increase one and decrease the other and you change it. Nature has delivered you this. This completely defies your biohacking desires to create a biohacking nightmare, which is that you have no control biochemically over this because it's literally the same chemical starting the inflammation and ending it.
Melanie Avalon: How does it decide what to do?
Chris Masterjohn: This is the thing. the chemical doesn't decide. Actually, this is very fascinating. The drug industry is largely driven by biochemistry because our culture is so dependent on pharmaceutical industry. As a culture, we prize biochemistry above other sciences. By biochemistry, this enzyme controls that and this thing controls that enzyme. If you block that enzyme or you block that receptor, you'll make this reaction happen or not happen. The case of resolution of inflammation is so fascinating because what it tells us is that physiology dominates, I think physiology is the right word to use here. Well, I'm going to use it this way. Maybe someone can critique me on it. That physiology dominates over biochemistry. What I mean by that is, the interaction between different cells and different tissues in the body is the thing that creates the resolution of inflammation rather than any chemical that is created by any enzyme or acts on any receptor. The biochemistry of an enzyme makes a chemical that acts on a receptor is completely subjugated to the balance between different cell types in different tissues and how they're distributed in the body.
What happens is, let's say, you have a wound, you get a cut or something. There are many immune cells that will now migrate to that wound to start healing it. Among those cell types are our neutrophils. This is like a puzzle that people are trying to work out and are nowhere near actually solving the puzzle yet. If they solve exactly what it is that determines the resolution of inflammation, that will probably be the biggest advance in inflammatory disease in decades. Solving this puzzle is what will fully shift the paradigm. When they can make this science usable in how inflammation is treated clinically, once that puzzle is solved, it'll basically be a new era of replaced the last, whatever. I don't know when they discovered the COX enzymes, but this has to be many decades ago. This is like a new century of inflammation treatment. But what the puzzle is looking like is the burden of neutrophils is one of the key signals that the inflammation has to start resolving. And so, it’s like there are ways of sensing that the work done at the wound is nearing its completion and now you can start the next stage. A wound healing is an exact analogy to--
With low-grade chronic inflammation, where the inflammation is not supposed to be happening, it's like, “Well, how do we replace that signal?” Because we don't actually have a clear work objective. We're not supposed to be inflamed right now. But if you look at what's happening at a more granular level, it's actually quite fascinating because there are some cells that make certain enzymes in a pathway, and other cells that make other enzymes in the pathway, and those cells have to be next to each other in order to make certain chemicals get produced. It's like prostaglandin E2 made from the omega-6 fatty acid, arachidonic acid using the COX enzyme that you inhibit with all your anti-inflammatory drugs, prostaglandin E2 will induce an inflammatory or a resolutionary, the resolution of inflammation state, depending on the other cells that are around and whether they're next to each other or not. It's looking like the resolution of inflammation is actually about the cycle of cells that need to migrate to the wound at different stages in order to engage in the first like, don't bleed to death phase, and then fix this mess phase, and then clean it up phase.
There are analogous processes of a viral infection. First, you're trying to make it not multiply, and then you're trying to destroy it, and then you're trying to clean up the mess. But from this, however, and this gets back to your question. I took the long way here. The first lesson there is that omega-6s aren't intrinsically inflammatory. NSAIDs don't make sense. The paradigm is now left NSAIDs behind to where they were based on the old paradigm, and they don't really do what they're supposed to do in the new one. Because NSAIDs are preventing you from making prostaglandin E2, which yes, it makes inflammation, but it also ends inflammation. The animal experiments that really suggest that's a bad idea, what they did was in multiple different models, they showed that if you create an inflammatory scenario for an animal, you get up to a peak inflammation and then it goes back to baseline. If you give them NSAIDs, they don't hit the high peak inflammation. They hit a lower peak of peak inflammation. But they also don't resolve it. Their peak inflammation is less, but they never go back to normal. What that tells you is that blocking the enzyme that creates the inflammation causes chronic low-grade inflammation. What that really tells you is that the epidemic of chronic low-grade inflammation, the cause of that appears to be the old wrong paradigm that formed the last half century of how people have been dealing with acute inflammation.
This is changing in other ways like under the old paradigm, people were always trying to treat any painful thing that came up. This is now very controversial in sports, but people would take NSAIDs while they were recovering from exercise, because there's post-exercise inflammation. And now, that's very controversial, because it looks like post exercise inflammation is good for you. It's good for your recovery. The old paradigm of inflammation, which is still dominant looks to me that it created the epidemic of chronic low-grade inflammation. By teaching us that we could control this one chemical by blocking this one enzyme to stop us from reaching the peak inflammation. It took us 50 more years to find out that that also prevents us from ever going back to no inflammation.
Melanie Avalon: In that situation, where so, we have this injury or something that would “require inflammation,” where inflammation would play a role. That's where the prostaglandins would come in and either create and/or resolve the inflammation. If you just live through that, and you're taking the pain pills the whole time, and you don't let the inflammation ever happen, does the event not resolve itself on its own? I know you said that prostaglandins are needed to resolve the inflammation. But does the event itself not heal and then we don't even need to worry about prostaglandins creating or not, or resolving inflammation?
Chris Masterjohn: Do you mean if you get a wound will you not heal the wound if you take NSAIDs, is that you mean?
Melanie Avalon: If you stop prostaglandins from happening, you're blocking that COX-2 enzyme with your NSAIDs. You were saying that they're needed to ultimately resolve inflammation, but they're addressing whatever's happening. That's where they would be creating or resolving inflammation. But do those things not go away on their own? Can you not just wait it out, why would you be in a perpetual state?
Chris Masterjohn: Instead of taking the NSAIDs or taking the NSAIDs? What are you asking?
Melanie Avalon: Taking the NSAIDs.
Chris Masterjohn: Well, I think the data would suggest that a lot of people who just take the NSAIDs wind up with pretty serious gut problems. Yeah, your headache might go away, but that doesn't mean that you don't wind up with autoimmune arthritis at some point.
Melanie Avalon: Yeah. What I'm trying to clarify is, the prostaglandins role in creating inflammation or resolving inflammation? But if they're just never there to begin with.
Chris Masterjohn: Look, so, these animal experiments didn't last forever. It's possible that rather than staying forever, it stays for 50% of your life or something. I don't know what that would-- If they let the animals live out until they died of natural causes, maybe it does return to baseline. But what they show is that, if you immunize an animal against its own collagen such that it'll develop autoimmune arthritis. If they get NSAIDs, they don't get as much swelling in their joints, but the swelling also never goes away.
Melanie Avalon: Okay, yeah. I'm thinking of it in two different situations like a wound situation, but it would be different if it was an ongoing--
Chris Masterjohn: Well, even with a wound, there's different levels of healing of a wound. So, I don't know—[crosstalk]
Melanie Avalon: Well, the healing never happened without the inflammation?
Chris Masterjohn: Some healing will happen, because you're not going to bleed to death. First of all, the resolution stage of healing a wound is not aimed at accomplishing the healing. It's aimed at clearing the inflammatory cells out of the tissues. That's important because inflammatory cells, I mean, they're inflammatory, but they also can be damaging. They migrate to the wound to fix it, but if you just dump neutrophils on healthy tissue, it's going to damage it. They make a lot of reactive oxygen species and they're not supposed to be hanging out all the time in your tissue. The real question is, whether the wound heals. Do you have chronic swelling or beneath the wound chronic damage to the tissues from a burden of inflammatory cells that never fully goes away? I don't know if there're any studies on NSAIDs and wound healing, but I would also note that wound healing isn't all the same. You can heal the wound with healthy tissue, you can heal the wound with scar tissue. There are multiple ways to heal a wound and scar tissue is the one you don't want. I'm not saying that blocking prostaglandins will cause scar tissue. I have no idea if that's been studied, but I'm just making the point that healing any wound is inevitable unless you die or get a severe infection. But you can heal a wound in a far from ideal way and that's how you wind up a scar tissue. I have no idea how NSAIDs might impact that, but I would be interested to see.
Anyway, with the omega-3s, one possible answer to chronic low-grade inflammation is that your body doesn't have the tools to fix it, to resolve it. What's interesting is that although omega-3 is playing no particular role in initiating inflammation, they play a very central role in responding to prostaglandin E2, which is made from the omega-6 arachidonic acid by also playing a role in resolution. You can imagine that if you do have enough omega-6 to go through that cycle, but you don't have enough omega-3, then your resolution, it's not that it won't happen, or can't happen, or has nothing promoting it. It's just that you're missing a core piece of the army of biochemicals that will make it happen. You're missing all the omega-3 derived pro-resolution compounds. As it turns out, DHA is the main participant there. EPA, early evidence was suggesting that EPA could only participate in the presence of aspirin although, there's now evidence that certain bacteria can also make EPA act pro-resolution. That might only happen under certain circumstances. For example, it might only happen in the gut, where those bacteria are present or in the case of a systemic infection when they would be present. I'm still conservative about using EPA for that purpose.
But EPA versus DHA, there's another problem with EPA, which is that EPA is a COX inhibitor. If you're using high dose fish oil, that's like taking an NSAID. DHA doesn't block the COX enzyme and it does participate in resolution. I think that the natural cycle, the dominant normal physiology involves relying on omega-6 fatty acids without anything obstructing their way, make prostaglandins, and then when it's time initiate resolution and DHA will become intimately involved in that. I'm not opposed to necessarily using EPA and aspirin in that case, but I think you're getting into a more pharmacological approach when you do that.
Melanie Avalon: So, does aspirin fall under-- we’ve been saying NSAIDs?
Chris Masterjohn: Yeah. Aspirin is interesting because it is an NSAID and yet, it does something different to the COX enzyme versus all the other NSAIDs. Most NSAIDs just block the COX enzyme. And aspirin, this is not true of food salicylates. it is only true of aspirin. Aspirin acetylates the COX enzyme, which does, yes, reduce its production of prostaglandin E2, but it shifts the enzyme into making the pro-resolution compounds. Aspirin is in a gray area where it does both. And so, it's the one over-the-counter anti-inflammatory that you could argue is pro-resolution, because even though it blocks the usual pro-resolution compound, prostaglandin E2, it itself substitutes for prostaglandin E2 in being pro-resolution. However, I would note that in the gut prostaglandin E2, it's not just a pro-resolution compound, it is essential to the normal state of producing tolerance to foods. I'm not comfortable with the lack of data on whether aspirin could contribute to food allergies. I do trust aspirin over all the other NSAIDs and way over acetaminophen providing someone doesn't have an adverse reaction to aspirin, which would usually just include like bleeding in response to it, but some people have aspirin-induced asthma and stuff like that. For people who tolerate aspirin, I do think aspirin in my view is the anti-inflammatory of choice because of its pro-resolution capacity. However, I'm not too happy with the idea of blocking prostaglandin E2 in general, especially, chronically all the time, because I do worry that that would contribute to food intolerances.
Melanie Avalon: There are two compounds that I always want to ask the guests about and I'm dying to know their opinion on. One is aspirin because I'm just haunted by the cost benefit of it. The second one, and maybe this could be our last thing. So, I want to be very respectful of your time. I want it to be rapid fire question, but NR versus NMN, what's your current thoughts on that?
Chris Masterjohn: I think that NMN is likely digested to NR if it reaches the intestines. I don't know much about the sublingual transport, but there's NMN transporter, it's probably mostly relevant before it gets into the stomach and especially the intestine due to the digestive process. My current belief is that NMN and NR are probably largely bioequivalent. I think that they're likely to have significant-- But I think that you're getting just by not being nice and deficient, you're getting most of the benefit. But if you're trying to increase NAD levels, I think you have a slightly better effect that you'll get from NR or NMN overtaking nicotinamide. But I think the two of them are largely going to be equivalent to each other.
Melanie Avalon: Even though the NMN would require a conversion to NR?
Chris Masterjohn: Well, there're two things. First of all, that's not an energy intensive conversion. Second of all, the enzymes that do that are nonspecific phosphatase is that are expressed at extremely high levels in the intestines. It's probably the case that you don't have much of a choice, but to digest NR in the intestines. You'll probably digest a portion of it to free niacin as well but the conversion of the NMN to the NR should probably be extremely high if not complete in the small intestine under most circumstances.
Melanie Avalon: There's this idea that NMN is shelf stable or it doesn't require refrigeration, but NR does. Is it more fragile, do you know?
Chris Masterjohn: NMN doesn't require shelf. On top my head, I don't know. Yeah, I'm not sure.
Melanie Avalon: Okay. Two last rapid-fire questions. Have you done an NAD IV?
Chris Masterjohn: No.
Melanie Avalon: I haven't either, but it's a lot of money to spend for something that apparently can be very unpleasant to experience.
Chris Masterjohn: I'm more concerned about the unpleasantness. I don't know what the cost is, but I stop at the unpleasantness.
Melanie Avalon: Unpleasantness, yeah. Do you know if there's an issue with NR wasting methyl groups like having a taxing effect because of requiring?
Chris Masterjohn: Oh, yeah, all niacin will tax methyl groups to some extent.
Melanie Avalon: Okay. Things to consider. Well, thank you so much. This has been amazing. I could ask you questions for ever, so, I will not. I really, really appreciate all of your work. For listeners, you have so many incredible resources on your website. What links would you like to put out there for people to best follow your work, get your guides, support you, all of those things?
Chris Masterjohn: chrismasterjohnphd.com/uncensored or follow me on my new Substack at chrismasterjohnphd.substack.com. Those links go to the same place. That's my newsletter. Everything else can be found from there.
Melanie Avalon: Awesome. Well, I will say, I have not subscribed for Substack, but I did recently to follow your Substack. That's what made me turn over. The last question I ask every single guest on the show and it's just because I realized more and more each day how important mindset is. So, what is something that you're grateful for?
Chris Masterjohn: I'm [chuckles] incredibly grateful that I have an audience of people that care enough about me to support me while I do what it seems is my greatest gift to the world, which is use my analytical brain to break down science in ways that people can use for their health. That's granted me an enormous amount of personal freedom, as well as fulfillment, and feeling like I'm doing what I was put here to do.
Melanie Avalon: Well, thank you so much. I cannot say enough how grateful I am for your work, and all that you're doing, and you're just helping so many people. This is amazing. I will continue to follow all of your content and hopefully, we can talk again in the future. But thank you so much.
Chris Masterjohn: Awesome. Thank you so much, Melanie. This was great.
Melanie Avalon: Thanks, Chris. Bye.
Chris Masterjohn: Bye.
[Transcript provided by SpeechDocs Podcast Transcription]