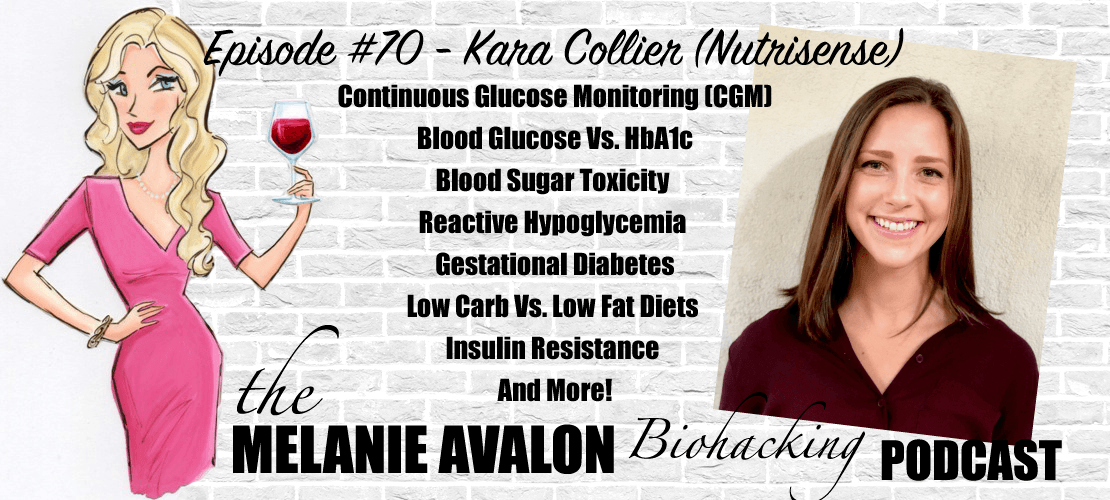
The Melanie Avalon Podcast Episode #70 - Kara Collier (Nutrisense)
Kara Collier is a Registered Dietitian Nutritionist and Certified Nutrition Support Clinician with a background in clinical nutrition, nutrition technology, and entrepreneurship. After becoming frustrated with the traditional healthcare system, she helped start the company NutriSense where she is now the Director of Nutrition. Kara is the leading authority on the use of continuous glucose monitoring (CGM) technology, particularly in non-diabetics for the purposes of health optimization, disease prevention, and reversing metabolic dysfunction. Kara oversees the health team and product development and has personally interpreted thousands of complex glucose datasets.
LEARN MORE AT:
https://www.nutrisense.io/
https://www.instagram.com/nutrisenseio/
https://twitter.com/nutrisenseio
SHOWNOTES
1:50 - Go To Melanieavalon.com/nutrisenseCGM And Use Coupon Code MelanieAvalon For 15% Off Select Packages
2:20 - Follow Melanie On Instagram To See The Latest Moments, Products, And #AllTheThings! @MelanieAvalon
2:40 - IF Biohackers: Intermittent Fasting + Real Foods + Life: Join Melanie's Facebook Group For A Weekly Episode GIVEAWAY, And To Discuss And Learn About All Things Biohacking! All Conversations Welcome!
3:10 - BEAUTYCOUNTER: Non-Toxic Beauty Products Tested For Heavy Metals, Which Support Skin Health And Look Amazing! Shop At Beautycounter.Com/MelanieAvalon For Something Magical! For Exclusive Offers And Discounts, And More On The Science Of Skincare, Get On Melanie's Private Beautycounter Email List At Melanieavalon.com/cleanbeauty! Find Your Perfect Beautycounter Products With Melanie's Quiz: Melanieavalon.Com/Beautycounterquiz
6:45 - kara's Background
10:45 - What Is a CGM?
11:50 - Prescription Requirements
13:20 - CGM History
14:15 - CGM Application
14:55 - How Does It Work?
16:50 - Measuring Interstitial Fluid Vs Blood
18:05 - Best Placement Of The CGM
19:05 - Accuracy of the CGM
22:20 - Calibration For true Values
24:05 - INSIDE TRACKER: Get The Blood And DNA Tests You Need To Be Testing, Personalized Dietary Recommendations, An Online Portal To Analyze Your Bloodwork, Find Out Your True "Inner Age," And More! Listen To My Interview With The Founder Gil Blander At Melanieavalon.Com/Insidetracker! Go To MelanieAvalon.Com/GetInsideTracker And Use The Coupon Code MELANIE30 For 30% Off All Tests Sitewide!
27:50 - What Is A Good Range For BG?
28:50 - Fasted Glucose vs hbA1c
30:50 - How Long To fast For fasted glucose?
32:00 - what is normal bG after eating? post prandial readings
34:00 - Peak glucose value
34:50 - Glucose Toxicity
36:35 - Insulin Resistant Readings
37:15 - shorter high glucose spike vs prolonged glucose response
38:35 - insulin resistance on low carb diets
41:10 - Pathological Insulin Resistance
42:00 - Testing Fasting Insulin
43:00 - High Glucose due to cortisol
44:50 - Is insulin resistance bad if markers are good?
47:05 - advanced glycation end products
49:25 - Longevity vs glycation
50:40 - communication pathways
53:30 - avoiding Pathological insulin resistance
58:00 - HCLF Diets
1:00:00 - Frequent Insulin Stimulation
1:03:05 - BiOptimizers: A Company Whose Mission Is To Fix Your Digestion! Get Their Full Spectrum Magnesium Supplement To Fix Your Magnesium Status, Containing All 7 Versions Of Magnesium!! Go To Bioptimizers.com/melanie And Use Coupon Code MELANIE10 To Save Up To 40% Off Select Packages To Get The Most Full Spectrum And Effective Magnesium Product Ever!
1:06:00 - reintroducing Carbs
1:07:35 - CGM During Pregnancy
1:09:35 - what causes gestational diabetes?
1:11:15 - breastfeeding effect on insulin resistance
1:12:10 - specifics of hbA1c
1:16:30 - factors that change hbA1c
1:17:15 - fructosamine vs hbA1c vs albumen
1:19:05 - reactive Hypoglycemia vs fasted hypoglycemia
1:25:15 - Digestive Enzymes effect on glucose
1:27:20 - how long do i have to use the cGM?
1:29:00 - trial options and recommendations
1:31:40 - Go To Melanieavalon.com/nutrisenseCGM And Use Coupon Code MelanieAvalon For 15% Off Select Packages
1:32:40 - how to interpret the data in the app
1:34:20 - the benefits of nutrisense
1:35:20 - access to a dietician
1:37:40 - do you ship internationally?: app only support?
1:39:05 - EMF exposure
1:41:15 - the future of nutrisense
TRANSCRIPT
Melanie Avalon: Hi, friends, welcome back to the show. I am so excited about the conversation that I am about to have. It's about something that I have been personally experimenting with for the past month and a half or so. It's been so fascinating. I am learning so much about my health, about monitoring my diet, about how food and fasting and things like that affect me. I've been telling you guys about it. You've been dying to hear my official interview and thoughts on the topic. So, that is what is happening right here, right now.
Friends, I've been using a continuous glucose monitor. Today, I am here with the founder of a company called Nutrisense, which is really doing incredible things and making continuous glucose monitors actually accessible to the general public because, we'll probably go into this in detail, but normally you would need a prescription and it's normally for people who have prediabetes, diabetes, things like that. So, it is actually a very valuable tool. I am so grateful for a wonderful woman named and I just learned how to say her name correctly, Kara Collier, for founding this amazing company called Nutrisense. Kara, thank you so much for being here.
Kara Collier: Yeah, absolutely. Thanks for having me. I'm excited to chat.
Melanie Avalon: I am, I have so many questions. What's really great is, like I said, I have been using one for about a month and a half now. I've seen what I can learn and I'm starting to see what I have a lot of questions about, but for a little bit about Kara. She is a registered dietician, nutritionist, and also a certified nutrition support clinician. She has a background in clinical nutrition, nutrition technology, and entrepreneurship. I think it's really wonderful when those things come together because when you have all of those skills and assets, they can come together to create amazing things like this company, because Kara herself became frustrated with the traditional healthcare system and started the company called Nutrisense, where she is now the Director of Nutrition. She's a leading authority on the use of continuous glucose monitoring, which is called CGM technology, particularly in nondiabetics for the purposes of health optimization, disease prevention, and reversing metabolic dysfunction.
Kara, I have so many questions for you. But to start things off, I did just tell a little bit about your bio, but I would love to hear in your own words, what did that look like? What was your journey like that led you to where you are today with having this interest and monitoring blood glucose, CGM, and forming the company, Nutrisense? Which, by the way, when did you guys start it officially?
Kara Collier: Yeah, we started taking customers and launched to the public about 14 months ago. So, a little over a year at this point. It's been an awesome journey so far.
Melanie Avalon: Were you in a beta period for a while before that?
Kara Collier: Yeah. About six months before that, we were building and testing, building and testing.
Melanie Avalon: Well, I should say congratulations, building a company like this is no small feat. That's incredible. What led to that? Did you just wake up one day with an obsession of monitoring blood glucose, what did that look like?
Kara Collier: The obsession has been there for quite a while now. But it really stemmed from my experiences working in the hospital system. As you mentioned, I am a registered dietitian, and I started my career working in hospitals, particularly ICUs. So, of course, this is where people are the sickest of the sick. What I was seeing over and over was a lot of people coming into the ICU with complications of preventable conditions. So, they're coming in because they need an amputation because of uncontrolled diabetes, or we need to put them on dialysis because of kidney failure. A lot of this is related to diet and exercise, and all the things we'll dive in today. It was just very, very frustrating to see all that suffering, unnecessary pain and time and expenses. When I really felt like, lot of those people didn't need to be there.
In the current system, the traditional health care system, which does a lot of things really well, but it doesn't do prevention very well. I felt it couldn't make the difference I was looking for in that system. Instead of trying to fight that system, I decided to make my own system that can help address some of these problems. From there, I really got to think like, “What is the root cause with all of these conditions we're seeing?” It really comes down to metabolic health and insulin resistance. That is so intricately linked to the top killers in the United States and globally, not just diabetes, but cardiovascular disease, cancer, Alzheimer's. All of these conditions can be linked back to our metabolic health.
In the goal of the 80/20 rule, biggest bang for your buck, really, I started to dive into glucose management as a metric we can focus on to make a big meaningful impact. I wanted to do that in this population that's not already multiple chronic conditions, so we can prevent them from getting there. So, that's really where it all started, and my interest is just seeing how it really works and how those last 10, 20 years of somebody's life can be full of pain and suffering when really we want that to maximize health span and you be able to enjoy your older age and not have all these medications you're on and procedures and complications. So, that's the ultimate goal here for me.
Melanie Avalon: I love this so much. The last interview I did was with Dr. Benjamin Bikman who wrote a new book all about insulin resistance, and it's just really mind-blowing. I love what you said about with prevention. What is one marker that we can look at pretty consistently that speaks to everything in a way? I know I'm saying blood glucose, but CGMs don't actually measure blood glucose. So, maybe that's something that we can go into. Actually, starting there, with actual-- the CGM, so that listeners can actually know what this device is. You just answered a question that I got a lot of questions about, like Katherine said, “Why should I use one if I'm not diabetic?” But to that point, historically, what are CGMs? When did they start being used? Why do they pretty much require a prescription? How can they be made available now? What are they doing? How are they different from blood glucose specifically?
Kara Collier: Continuous glucose monitor or CGM is a small device that essentially you can put on at home and it goes on the back of your arm for the most part, different brands have them where you can place them in different places. But essentially, it's a way to attach this device to your body so you can get 24/7 glucose readings. Whereas if you have a glucometer at home, and you're pricking your finger, that's just a snapshot in time. So, instead, a CGM is sort of like a movie of what's going on inside. It is considered a medical device, so it does require a prescription from a physician. I believe this is an unfortunate thing, and this is specific in the USA. In other countries, in Europe, in Canada, in Australia, you can get these devices over the counter, you don't need a prescription.
Melanie Avalon: Oh, really?
Kara Collier: Yeah, in the US, the FDA has the legal authority to regulate both drugs and also medical devices. Essentially, they get to decide what's a medical device and what's not. That's really what it comes down to. As FDA said, the CGMs are medical devices, so they regulate them and they say it needs to have a prescription, where something like a glucometer that you're actually drawing some blood from your finger is not a medical device, according to the FDA, so you can buy it over the counter. So, that's really what it comes down to, which is unfortunate because it limits so many people from this very valuable data. What we're doing is we're trying to allow this to be easily accessible to as many people as possible.
Historically, these devices were really only used for insulin-dependent diabetics. Type 1 diabetes is where you don't produce insulin, that's the main market for CGMs. Type 2, that's more of a lifestyle controlled or lifestyle-caused diabetes. Really only about a third of type 2s are even wearing CGMs. Not even all diabetics are wearing them.
But these devices have been around for about 20 years, and they've come a long way since then. So, we really anticipate, they're just going to keep getting better and better. When they first came out, they only lasted three days. And now, the sensor we use, the Abbott FreeStyle Libre, it lasts 14 days. Essentially, put this thing on in the back of your arm. For those who are worried and asking because I get this question a lot, it does not hurt. You can put it on at home, you don't need your physician or anybody else to put it on for you. I always describe it as an easy button. It comes in this applicator and you push it to the back of your arm and just push the easy button, and then it's in your arm. It's just this little disc, you can shower with it, work out with it, do your normal activities. And if you're ever curious about your glucose values, you just have to scan your phone over the device, and then you can see an updated view of your glucose. In a nutshell, that's how it works and how it's regulated in the US.
Melanie Avalon: Yeah, I will speak to putting it on. So, it's funny because I'm a “biohacker.” I feel I'm often injecting, sticking myself with things all the time, like glutathione and blood pricks. I'm not scared of it at all. Like you said, it lasts for two weeks, so when I got my first sensor, the applicator looks intimidating, because you can see the needle that it uses to put it on. Friends, you don't feel it at all. It's almost shocking, and I've done it three times now. Like you said, it is an easy button. I put it on, I was like, “Wait, what?” You don't even feel it.
Kara Collier: Yeah, it's completely painless.
Melanie Avalon: Yeah. Some questions about how it actually works. Well, I love what you said about the movie metaphor because I think the biggest epiphany that I've had about all this is just, if we go get our labs drawn and we see our blood glucose at that moment, if I had gone in five minutes later, or maybe jumped or coughed or thought about something, it's crazy how much it can vary. Maybe this probably varies by person as well. I'm sure maybe some people's varies more than others. I've just realized, wow, one marker at this one time with a blood draw, or a prick or a blood glucose monitor is so different from seeing it, how it changes 24/7. So, listeners, I mean, it's mind blowing, honestly. As far as how it actually works, it's not measuring your actual blood, right?
Kara Collier: Yes, that is right. It is where-- the glucometer that your audience may be familiar with, where you're pricking your finger, you're drawing blood and it's measuring your glucose values in your blood. Whereas CGM, because this is part of what makes it so painless is, it's inserted just barely below the skin. And so, it has this little flexible microfilament that's measuring glucose values in your interstitial fluid, which is just the fluid between cells. So, it's not even going to the depth of blood. And that's why you don't feel it and it's super painless. And so, this is a little bit different than your blood glucose values. But it is still essentially like glucose in your body, it's just in a different compartment. If we think about like-- let's say I just ate a candy bar, glucose molecules from the candy are going to get broken down into my bloodstream first, and then it's going to diffuse into my interstitial fluid. Eventually, that glucose ends up there and regulates, but it's a slightly different area to measure, if that makes sense.
Melanie Avalon: The blood glucose in your blood, and then there's your cells, and there's this fluid around the cells, so does the blood glucose always have to go through the fluid, and then it enters the cell-- like the potential pathway of blood glucose, is the interstitial fluid like a passive ocean around the cell that the blood glucose passes through?
Kara Collier: Yes. It is like passive diffusion. Eventually, it will end up there, but that's why if you're measuring, the glucose level and the blood in your finger, and your interstitial fluid in your arm, they're never going to be perfect matches. We call them unicorns if they perfectly match, because you're not measuring it from the same area. Just like if you took a finger prick from the blood value in your hip versus your finger, they're not going to perfectly match either, because you're just drawing it from different areas. Whereas the CGM is measuring that interstitial fluid, and it does have a little bit of a lag time. So, your glucose might spike more in your bloodstream like 15 minutes after eating, and it might show up in the interstitial fluid 30 minutes after eating because there's a little bit of a lag time due to that diffusion.
Melanie Avalon: When they say to put it on, they recommend putting it on a fatty area. Wouldn't you want to put it on a less fatty area because it would be closer to the bloodstream?
Kara Collier: Yeah, that's a good question. We have tested this, and since the devices are originally made for, or the target audience is a type 1 diabetic, which are often children, what they have noticed, the manufacturers of the devices, is that with children who are really lean, they don't have a lot of fat, they tend to have more inaccuracies with the data. It seems that if it's not-- so that fat really helps it to be bathed in that interstitial fluid. I guess there's more there. I should probably dive into the nuances of that. But I do know that accuracy tends to be better if we put it in that fatty area because that's where it's been tested for. That's a good question. Some people who are more lean, we tend to have to calibrate it a bit more. We can dive into accuracy if you want to because that's a common question I know comes up with the CGM devices, but the placement plays a role in that as well.
Melanie Avalon: Okay, yeah, that is so interesting, because often they'll talk about circulation to fat stores and things like that. So, I was just pondering it. Since we are talking about the accuracy, what does affect the accuracy? I've done three FreeStyle Libres now, and I have been checking them against my own blood glucose-- Sorry, everything's [unintelligible [00:15:18] my head, blood glucose monitor. And so, the first one seemed to be-- it was usually high by about 10 to 15 points. The second one I ran, talking about unicorns, I mean it pretty much would match up., it seemed like a unicorn. The one I put on a few days ago, it actually seems to be high by about 20 to 30. In those situations, is the device going to be accurate for the relative changes and then you can calibrate it to the correct number? What's going on there? How can we perfect accuracy to the best that we can?
Kara Collier: That's exactly right. So, the sensors, and this is across the board. There's three main companies that make these. There's Abbott, who makes the FreeStyle Libre that we use. There's Dexcom, and then there's a brand called Medtronic. For all of these CGM devices, they do have fluctuations in the absolute accuracy. Meaning that the number value itself could be a little bit higher or lower than true value, but the precision tends to be spot on. Those changes in glucose, the trends, the shifts in your values, that is very precise because they're FDA regulated. FDA tests all these brands and has declared that they're accurate enough that those who need insulin dosing are able to dose off of these devices. That precision, the change in glucose is shown to be very precise.
The absolute value, like you said, what we like to do-- and the app that comes with the FreeStyle Libre does not allow you to calibrate yourself. So, if it's off, you can't do anything about it, which is obviously frustrating. If you can see it's off, you want to be able to adjust the values, but the app that comes with the Libre does not allow you to do that. So, in our app, we do allow you to manually calibrate. Typically, we recommend to do it in a fasted state just because of the difference, the lag time between blood glucose values and interstitial values, it's easier to match it up in that fasted state. So, if you check on your glucometer in the morning after you wake up and move around, and it's reading 75, and then your CGM reading at that same exact time is 85, you can adjust that in the app to calibrate it 10 points, and then it'll adjust it for the whole sensor, and you don't have to check it anymore. We typically recommend adjusting it once and then letting the trend speak for itself from there, if that makes sense.
Melanie Avalon: Some more specifics to that, because you said the precision is accurate. I know you said the fastest state would be the best time, but would a person want to maybe wear it a certain amount of time, check at a certain amount times and notice that it seems to be off before making that calibration change? Or is it fine to just calibrate at any time?
Kara Collier: Yeah, the sensor is self-calibrating during the first 12 to 24 hours. When you first put it on, it's doing its internal calibration to try to get it as close as possible to true values. We usually recommend-- if you have a glucometer at home, if you have something to double-check, doing it on that second day in the morning when you're fasted to see how it compares. And that's the best time to make an adjustment. From there, you're usually good to go. I don't want people to necessarily have to prick their finger over and over, it should be adjusted for the whole 14 days if you just do it that one time. Of course, you could continue to spot check and get it as close as possible. But the glucometers themselves have a little bit of variability. I don't know if you've ever noticed this, but sometimes I'll take a value on one finger versus the other finger and they're different. So, those devices aren't perfect. The calibration and making the adjustments is to try to get an approximation and get as close as possible.
Then, we really want to focus on the trends that the CGM is providing us because that's where infinite insights lie. You can see was my fasting glucose value yesterday higher or lower than today when I made X, Y, Z adjustment? How much did my glucose rise or fall after a meal? All of those trends and shifts in glucose are what we really want to glean the insights from.
Melanie Avalon: That's just so helpful. The reason I wanted to really talk about it was I want to make sure people when they get their sensors that they do get it, calibrate it up to their body because we would not want to have the-- like a person making maybe unnecessary changes or drawing conclusions when it really is just calibrating the device would get them on the right path?
Kara Collier: Exactly. Yeah. We'd like to mention it, because everybody gets a dietician when they start with us, and we'd like to mention it at our first contact. Just in case maybe that's part of what's going on, I would say 50% to 70% of people don't have to adjust the sensor at all, because it's within five or so points or pretty close. But we want to make sure that you're at least aware of that. Yeah, we're not making incorrect conclusions about your data. And that's why it's important to have real people there as well, so we can talk through that if anyone's confused.
Melanie Avalon: Like I said, I think the first one probably was fine. It was a little bit off, but it was fine. Second one was spot on. This one, I'm definitely going to calibrate right after we talk because I'm fasted right now. The actual, what we're monitoring, so the blood glucose levels, got a ton of questions about that. I have a lot of questions. Becky, for example, says, “What is a good range to be in? What number should we be looking for? What is the normal “good blood glucose levels” and do you agree that the conventional standards are what we should be aiming for?” Just to give a terminology and a language to all of this, what are those ranges?
Kara Collier: I can walk through what's normal in traditional settings, and then what we consider optimal from our view of really looking at the lens of prevention and longevity, and not just normal. If you were to just go to your doctor's office, and you were going to check and see how your glucose values looked, you would probably get two metrics. One would be a fasting glucose value, and that's on your standard panel, and then the other would be a hemoglobin A1c. With the fasting glucose value, it's exactly what it sounds like, it's your glucose in a fasted state. When it's just on the regular lab panel there, of course, it's just a snapshot in time. As you noted, when you wear a CGM, you realize that your glucose fluctuates quite a bit. One day of bad sleep or some stress, or maybe you've got some adrenaline going on, because you're under pressure or something, and that fasted glucose value could be totally different than it looks the day before.
The unfortunate thing about just getting it from a lab is that you're only seeing that small snapshot in time. The lab is going to tell you if your fasting glucose value is under 100, that that's perfectly healthy, where we're really shooting for a fasting glucose value between 70 and 90. And that buffer zone of 90 to 100 would be a little bit of a yellow flag, raise an eyebrow, because there is a lot of research that shows fasting glucose values above 90 are an independent risk factor for increased risk of cardiovascular disease, diabetes, anything related to insulin resistance. We start to see that risk increase in those higher fasting glucose values. With that metric, we're really looking for 70 to 90. The nuance that some people who are on a more strict ketogenic diet, they might have a fasting glucose value below 70 and feel perfectly fine, and that's okay too. We're really making sure that you don't have symptoms of hypoglycemia, and then it's okay. So, that's fasting glucose.
Melanie Avalon: What is qualified-- Because when the audience is a lot of intermittent fasters, I think the definition of fasting can be-- what is considered a fasting glucose? How many hours after eating?
Kara Collier: Yeah, and that's a good question. Technically, again, if you're going to a lab, they're going to say you need to be fasted for at least eight hours for that to be considered a fasting glucose value. But if you think about physiology, we tend-- in a healthy system, so not somebody who's showing metabolic dysfunction or insulin resistance, we start to see people shift from that post-absorptive state where you're metabolizing food, you're stimulating all these different pathways, you tend to shift to more of the fasting pathways at about three to five hours after eating. For me, if you ate and then went to sleep, and we're looking at your overnight glucose values, I'm looking at more starting at three to five hours after eating depending on how big that meal was. If you ate 2000 calories, it's going to take a little bit longer to be in more of a fasted state than if you ate 40 calories or something. Technically, eight hours, but I'm looking a little more lenient at that.
Melanie Avalon: Lenient, meaning it's dependent on what you ate before?
Kara Collier: Yeah. It's not just that I want to see glucose values around 90 eight hours after eating. I also want to see it closer to three to five hours after eating depending on what the meal looks like and what the situation is essentially.
Melanie Avalon: Okay, gotcha. And then after eating, and I guess this would probably depend massively on what you're eating. I'm assuming your insulin sensitivity, things like that. So, after eating, what is a “normal blood glucose response?” I'm personally haunted by, fascinated by the concept of area under the curve. Maybe you could talk a little bit about that. Is there a difference or a benefit or a detriment to higher spikes that go down quicker, so that there's less “area under the curve” compared to lower spikes that might actually stay raised a little bit longer? So, there's a larger area under the curve. What is a normal healthy response to a meal? What is this whole area under the curve business?
Kara Collier: This is where I think wearing a CGM is just so insightful because you really cannot get this information with any other metric. If you're using a glucometer, you can check your glucose value like an hour or two after eating. But, again, you might miss the whole curve, you might miss the nuances of what that postprandial response looks like. So, you really can only see this with a CGM. There's a lot of things we want to look at, at a meal. So, the first thing we want to look at is how high does your glucose value go? What is the absolute peak? Interestingly, again, going back to the idea of traditional medicine versus optimal health, nobody-- World Health Organization, American Diabetes Association, they do not recognize peak glucose value as something of significance. They're looking at the postprandial state, just what your glucose is at the two-hour mark after eating. So, that's the only thing they're looking at.
They're saying, if two hours after eating, you’re 140 or less, then that's okay. We do not go by those rules, because we think there's a lot of convincing research to say otherwise. With that peak glucose value, we want to stay below 140 most of the time. When we spike above 140, research shows that we start to see-- and this is, again, this is about repetition. So, if you have one spike to 140, every once in a while, that is no big deal. Our bodies have systems in place to take care of that. What we don't want to see is you hitting 140 every single day from your standard meal that you eat every day. Then, that's when we need to do some tweaking. We don't want to see repeated exposure above 140 because that can impair beta-cell function, that can decrease our insulin sensitivity over time.
There's this idea of glucotoxicity, so a glucose value in the bloodstream at a certain amount at any point in time, can be damaging to our endothelial cells. So, these spikes are actually independent risk factors for cardiovascular disease, which is again, why monitoring glucose is so important, not just to prevent diabetes, but for all these other health conditions that so many people are affected by. When you have that spike, it damages the endothelial cells of your blood vessels, and then that causes an inflammatory reaction. Essentially, the body needs to send out some inflammatory cytokines to clean up the damage, it releases some oxidative stress. And this can cause atherosclerosis because of the damage to the blood vessels and this inflammatory process that's required to heal it. So, that's when repeated abuse-- Repeated exposure above 140, is when we get stuck in this feedback loop, where that short-term damage can't be corrected because we're doing damage again before we're able to completely recover.
So, that's a long-winded answer about maximum glucose value, why we want to stay below 140 most of the time. With that being said, it is very common-- let's say you eat a huge carb-heavy meal, maybe you drink a large soda, your glucose is probably going to go above 140. And that doesn't mean you're insulin resistant, it just means that you had a lot of sugar that you just consumed. Whereas if you have a large soda and you go above 180, that's when we start to have a red flag moment for potential insulin resistance. Above 180 is when that is an abnormal response where glucose is getting higher than it should in a healthy metabolic system, even to a high sugar load. We really want to stay below 180 all the time. We don't want to see it get hit that value. That's when maybe we need some work to be done on insulin sensitivity, but then we want to stay below 140 most of the time for optimal health outcomes and preventative health. So, that's one metric of the postprandial response.
Melanie Avalon: I love this. This is so fascinating. Can I make up a hypothetical situation? I'm just trying to understand this. It sounds sort of the difference between like acute intense stressor that could potentially damage you with the spikes, compared to a chronic stress. If it's high, but not too high, but for a longer period of time. Say, if you not a person randomly can pick this, but say that there was two situations, like one person who goes up to, like 140, or maybe a little bit above, but then goes down pretty quickly. 140, and then they're back to baseline. Let's say two hours later, compared to a person that only goes up to 120, but they stay there for five hours, like between those two situations, is one preferred?
Kara Collier: Yeah. There may not be a right answer to this question, but based off of my clinical experience and research I have read, I would prefer to see the person who spikes high but comes down quickly, rather than the person with this prolonged glucose response. I would find that more detrimental in the long term.
Melanie Avalon: Okay. I've been really fascinated by this question for a very long time. I'm sure, like you said, there's not really one right answer but it's definitely really interesting to think about. Especially what about people who seem to experience on low carb diets, a sort of physiological insulin resistance? It might not be that, I know, there's a lot of terminology that people throw around. Some people call it glucose sparing, I think, Paul Saladino calls it glucose sparing. Dr. Bikman was calling it glucose-- He had another word for it. Basically, this idea of people on lower-carb diets who seem to experience higher fasting blood sugars, not like crazy high, but maybe 100s, 110, what do you think is going on there?
Kara Collier: This is something we see quite a bit where the reason people are coming to us is they're like, “I've been doing ketogenic diet for five years, and my fasting glucose values five years ago are 75. Then they were 85, and 95. Now they're 115,” which is prediabetic, diabetic levels. They're like, “What the heck is going on? I haven't changed anything else.” I see this a lot. And is this idea of physiological insulin resistance, adaptive glucose sparing, whatever you want to call it, but essentially, if you think about it, the body is super adaptable. If you are never giving it glucose, carbohydrates from the outside source, you're never eating food that has glucose in it, it's going to start adjusting its internal system. What's happening is that over time, fasting insulin is going to lower because it's not needing insulin as much because you're not ever giving it carbs. And then peripheral insulin sensitivity decreases as well, because you're not needing to use it. Then the body is raising its endogenous glucose production.
We're making more glucose from the liver via gluconeogenesis because we do have glucose-sensitive organs, like the brain that need a constant and steady flow of glucose. If you think about it just from adaptive ability standpoint, the body's like, “Well, I need to make sure I always have glucose coming in, and you're not giving it to me from food. So, I'm going to make sure I'm always producing a little bit extra because I'm not getting it from the outside source.” What happens is that fasting glucose raises.
The first thing I want to check in this situation is what are your insulin levels, and somebody who has pathological insulin resistance. So, this is what's associated with diabetes and cardiovascular disease. This is where all the research associated with elevated fasting glucose values. These people have elevated insulin levels as well because they have pathological insulin resistance. If you're someone coming to me long term keto, glucose is rising, let's check your fasting insulin. If your fasting insulin is 2 or 1.5, because it's been lowering over time, and your fasting glucose is 115, it's much less concerning than the person who has a fasting glucose of 115 and a fasting insulin of 20 or 30, or 100 because that shows me that your body's pumping out insulin, but not responding to it. Whereas in long-term ketogenic person, you're no longer pumping out as much insulin, so your body's increasing glucose on its own. Does that make sense?
Melanie Avalon: Yes, I love this conversation so much. My obsession is, I don't know why I'm obsessed with gluconeogenesis, but I actually did just get my fasted insulin tested for the first time because I was feeling intuitively, like I was building up this psychological insulin resistance that we're talking about, having done a lot of low carb and things like that. It was really inspiring because I went to see my endocrinologist. And she suggested, as she was like, “We could test your fasting insulin.” And I was like, “Yes.”
Kara Collier: That's awesome. You have a good endocrinologist.
Melanie Avalon: I know, I was like, “This is the best moment ever.” I was happy to see because, like I said, I was researching insulin, and it seems that below, I don't know what your optimal level would be. But I read that below six was pretty good for fasting insulin, and mine was 4.5. So, that totally makes sense. For listeners if you have these high blood sugar levels in your bloodstream while you're fasting or while you're doing low carb, if there's a lot of insulin, clearly the insulin is not doing its job, because the blood sugar is still there. But if the insulin is low, and the blood sugar is high, there's not insulin present, to be lowering it.
Kara Collier: Exactly. Then it's more of a natural adaptation. One caveat I will say is that there's another reason that glucose-- especially in the fasted state could rise, and your insulin is also low. And that would be if for whatever reason, you have a lot of cortisol pumping out. So, maybe you're just somebody who doesn't sleep very much, or you're somebody who's under a lot of chronic psychological stress, or you actually have some sort of cortisol issue. That cortisol basically is our stress hormone, it's our fight or flight stimulation. And so this hormone if we're excreting more amounts than normal, it's telling the liver to make more glucose as well. So, that's also stimulating gluconeogenesis, because your body thinks it's under stress, it thinks it needs extra energy to fight off a lion or run for your life. And so, your body's pumping out more glucose, and it's actually decreasing cellular insulin sensitivity so that that glucose stays in circulation, because that's how we have evolved to function.
And, of course, in our modern environment, this is a bit of a mismatch. This is an unfortunate situation where we have a lot of stressors in our modern environment, and our body is responding in this way, that's not actually beneficial anymore. So, that's something else-- if you see your fasting glucose, rise your insolence in a good level, do a little check and try to assess, “Am I stressed?” “Am I getting out in nature?” “Am I seeing sunlight?” “Am I taking time for self-care?” “Am I sleeping enough?” Both deep sleep and sleep quantity. Do those questions as well. If you feel like you're in a good place there, then it might just be this natural adaptation.
The question everybody asks is physiological insulin resistance. We've checked the box that insulin is good, we've checked the box that you're not overstressed. Then the question is, “Well, is this a bad thing? Should I be worried about it?” This is a question mark in the research. If anybody says confidently, “Yes, it's a bad thing,” or, “No, it's not a bad thing.” They're lying, because we don't know, but I'm going to make the guess that it's probably fine. It's probably a natural adaptation. It's not dangerous in the way that high glucose and high insulin is, but it has a few implications. One is if you're somebody who then wants to have a big load of carbohydrates every once in a while, maybe on the weekend you want to be able to eat whatever, you're going to have a much higher glucose response than somebody who regularly consumes carbohydrates. This is due to that peripheral insulin resistance, it's temporary.
In those moments, you might have glucose excursions that are way, way higher than somebody who doesn't have physiological insulin resistance. So, if you want that flexibility to sometimes have carbs, and sometimes not, then you might want to work on reversing the physiological insulin resistance. This is the idea of metabolic flexibility. You're flexible to both, utilize glucose as a fuel and fat as a fuel. If you're somebody who you're like, “I love being keto. Carbs don't tempt me. I don't want to have a big carb meal every once in a while,” then it's probably not a big deal at all. I don't really see a problem with that rising glucose, if everything else is in good place.
Melanie Avalon: Just to clarify, I know this is your opinion, and just so nobody has to hold you to it, but not seeing a problem with it, that would be fasted blood sugar levels of approximately what during this situation?
Kara Collier: Yeah, I've never seen it go much higher than that 115. And that's people who have usually been very strict ketogenic diet for at least five years. So, this is long term adaptation. I've never seen it rise above that. If I did see somebody who is significantly higher than that, that would raise an eyebrow as well. It's just been outside of the pattern of what I've seen, but for the people where it's hitting those upper threshold of 110, 115, but we've checked all the other boxes and they want to stay strict keto forever, I'm okay with that, for the most part.
Melanie Avalon: Have they done testing on at what blood glucose level, glycation is more likely to occur in the bloodstream? Is it past that 115-ish, 120?
Kara Collier: That's a really good question because our research is not great on this. This is the big link between longevity and glucose is this glycation. So, I'm sure your audience is familiar with advanced glycation end products dubbed as age, which is very appropriate. This is essentially like-- if you have too much glucose in the bloodstream, you're caramelizing proteins. Hemoglobin, that's hemoglobin A1c. If it has too much sugar on it, you're essentially glycating it, and that's why you might have a hemoglobin A1c of 10%. That's a problem as opposed to something at 5% is normal amount of glycation on a hemoglobin molecule.
When we caramelize these proteins too much, they damage the cellular functions and limit things like DNA repair and structural integrity. This can speed up our epigenetic clock. That's one of the proposed mechanisms of the link between longevity and glucose control. A lot of these studies, they're relatively high glucose values where we're seeing this glycation. That's another thing where I'd also want to see in somebody who has this physiological insulin resistance, and it's really getting up there. I'd want to see that your average glucose is at least around 110 or lower.
A lot of people with physiological insulin resistance, their overnight glucose values will be the highest of the 24 hours cycle. While they're sleeping, it's that 110, 115. Then when they wake up and start moving around exercising, walking, it's dropping down usually to the 80s, 90s. Average glucose value overall is closer to about 100, which is very healthy and normal. If you're never dropping down and your average is exceeding 110, that's when I would start to get a little bit concerned that maybe you just have too much circulating glucose in your system at all times, that could then really stimulate this glycation of all these different proteins.
Melanie Avalon: I also wonder if there's a context of higher glucose in a fasted state, which presumably would probably have a lot of anti -inflammatory signals going on with that, compared to that exact same blood glucose level in a fed state, which probably looks very different as far as sirtuins and all of that. I wonder as far as the glycation potential, if that does provide a little bit of a safety net, I don't know.
Kara Collier: That's a good point. If I have a customer who's like, “My ultimate goal is longevity and prevention, and I want to be just the absolute healthiest I can be.” Then for that person, if I'm seeing this going on, I would say, “Let's try to correct the physiological insulin resistance.” So, it's really meeting them where their goal is. If it's somebody else, who they're like, “I just want eating to be simple. And it's simple with keto, and I feel good, my energy is awesome, and I don't want to change that.” Well, it might not be worth it, because it's just so unknown. If it's me, personally, I don't want to see the physiological insulin resistance because I really want to be metabolically flexible and be able to use both fuels. I don't want to feel I can't eat carbs ever. So, that's just my personal preference is I want that freedom with my macros.
Melanie Avalon: Question about the communication pathway that's going on in the body when this is occurring, because I'm assuming, we've got the bloodstream with the blood glucose. We've got the liver potentially creating the glucose from with gluconeogenesis. The brain, the pancreas, which can put out insulin. How do they all talk to each other? Is everything looking at the bloodstream and reacting to that? Is the brain telling everybody what to do? What does that communication pathway look like? If a person's blood sugar goes low, did the liver directly sense that and releases glucose and a fastest day? Or does the brain sense and tell the liver?
Kara Collier: It's typically the brain sensing these things and then sending out signals via hormones. So that's where hormones are really, really important because they can connect all the different organs to do the things they need to do, and they can be the messengers. The brain is typically sending these messages. In the instance of your glucose is starting to dip low, your brain recognizes that, and it stimulates glucagon, which is the opposing hormone to insulin. Glucagon stimulates pathways to raise your glucose values to an appropriate level. We're always in this ying-yang between insulin and glucagon and finding that perfect balance.
Your body is always looking for a perfect homeostasis with glucose. That's where I also find glucose to be such an interesting metric to monitor because it's a vital sign. Your heart rate is always fluctuating a little bit and your body's constantly trying to keep it in this certain range depending on what's going on. It's the same with glucose. Your body's constantly trying to raise it if you need to fuel an exercise, or lower it if you're pumping out too much, or if you just ate a bunch of carbohydrates or something. So, it's always adjusting to what you're eating, your fasting, your stress, your sleep, your exercise, and it should be fluctuating fine tuning.
There's actually really interesting research to show that a healthy metabolic system is constantly fluctuating all day, like up and down 5 to 10 points. So, you go from 100 to 95, to 105 all day, where an unhealthy metabolism, unhealthy glucose system is flatline. So, it's a gradual rise or gradual fall, but you don't see these little nuance fluctuations. Those little nuance fluctuations are showing that your body is constantly adjusting and fine tuning really precisely depending on what's going on in the system and which hormones need to be pulled on more than others.
Melanie Avalon: That's really reassuring to hear. That's a good. You're speaking about with the physiological insulin resistance. If there is a person who is not the type that wants to be keto their whole life and actually does want to eat carbs, practically, how might it look like that they could address that because Gabriella, for example, she said, “How can one get down the blood glucose levels to physiological insulin resistance? What is the appropriate blood glucose baseline to avoid getting into physiological insulin resistance? What strategies to avoid this if you still want to eat low carb? Should you eat carbs at every meal, or occasionally spike insulin with good carbs one or two days a week?” One of the amazing things about it, we can dive into this a little bit more. The amazing things about the Nutrisense app is you actually can work with health coaches who can coach you through and help you out with tackling the levels that you're seeing. What might that look like for somebody who is low carb, but they do want to eat carbs? What type of things might they experiment with while wearing their CGM and working with their Nutrisense app?
Kara Collier: If you are showing the signs of physiological insulin resistance, and you're really wanting to be more metabolically flexible to both carbs and fat, there's a few different tactics we can try. The first one is something where it's maybe more of a cyclical keto. You're adding in some carbohydrates at targeted times. This is for somebody who maybe they want to sometimes be in ketosis and sometimes not. Again, it's really hard to generalize an exact amount of carbohydrates and when that would be best to consume because I really can't emphasize enough how different we all are, and that's exactly why I think this data is so important, because everybody responds a little bit differently. And it takes a little bit of experimentation and trial and error. Having that data helps speed up that experimentation process. You can see right away, that's not working, this is working. And you can find a plan much faster than if you didn't have any data to reinforce your experimentation.
For many people, it can be just titrating carbs up just a little bit and it can make a difference. We usually start small and work our way up. Let's say right now you're eating 20 grams of net carbs a day, we can try 40 grams net carbs and time that carbohydrate after an exercise or after a walk, timing it with movement to help avoid a big spike as you start to acclimate to carbohydrates again, but that might just be enough, 20 extra grams might be enough to stimulate your body, I'm getting glucose from outside, I don't have to make this adaptation anymore. So, that's one of the first things we'll try. It's just titrating carbs up, timing it around exercise and see how those overnight values change.
Another thing we like to really emphasize is making sure you're doing some strength training and making sure you're physically active because in general, the more lean muscle mass you have, the lower your fasting glucose are going to be and the more enhanced glucose tolerance you have. I do have a handful of people I can think of that are like my body builder types. I have several examples of people who've been doing ketogenic diet for five plus years and they are very strong, they have a lot of muscle mass and their fasting glucose is 70 or 80. They never ever saw this adaptation occur and it's always with people who have more lean muscle mass. It's just because your muscles are such a huge sink for glucose. They want to utilize glucose, that's where our glycogen is stored, the liver and the skeletal muscles and your liver can only get so big, we don't want it to get bigger than it supposed to be. If you have more glucose storage space in your muscles, that's going to help with glucose tolerance and getting glucose out of the bloodstream. So, using those muscles, building those muscles up is really helpful for this as well.
The third tactic typically, it's really focusing on adding in some carbohydrates, focusing on muscle mass, and then also fasting. So, really making sure that that's dialed in, because that can help your body learn to tap into these endogenous glucose stores and figure things out. A lot of this is just playing with their eating window. Again, everyone is different of when the optimal time to eat is, but we can tweak that. I've seen that alone also help bring down those fasting glucose values.
Melanie Avalon: I'm so excited that you have so much experience with seeing so many people trying different diets and what it does to their levels. I've had on the show, Cyrus and Robbie, who wrote Mastering Diabetes, I've had Dr. Doug Graham of 80/10/10. What have you seen with clients or patients on high carb, low fat diets that actually are low fat and their levels? Have you seen trends with that? Have you seen that to be beneficial for some people and taking charge of their insulin?
Kara Collier: Yeah. I have seen many people try this, and that is part of the beauty of this. When we first started, it was like the wild west of trying to figure out what's normal versus abnormal of glucose data and non-diabetics. But now that we've seen thousands of people, we have these unique insights, but we have seen people do the very, very low fat, high carb. Robbie and Cyrus, if anyone's familiar with their plan, we have had people try that, and it is very interesting. Essentially what they are trying to prove is that, if you eat a lot of carbohydrates, you're going to increase your insulin sensitivity. And that is certainly true. If we think about glucose tolerance and insulin resistance, there's two sides to the coin. There's how much insulin you're putting out, and then there's how sensitive are your cells to the signal from insulin. That's the thing where if the physiological insulin resistance, if you're never giving your body carbohydrates, we decrease our insulin sensitivity at a cellular level, because we don't need it as much, and so that's physiological insulin resistance, where if you're giving your body a lot of carbs all the time, your cells become really insulin sensitive because it knows it needs to really pull on that pathway, because it's having to use it a lot.
The problem I have with a long term, really, really low fat, really, really high carb diet is that there's the other side of the coin, which is how much insulin you're stimulating. Insulin is stimulated for a lot of different reasons. But the primary stimulation of insulin is because glucose is rising. If you're eating a lot of carbohydrates at multiple meals in the day, you're putting out a lot of insulin. I do worry about-- especially in somebody who already has insulin resistance, which is what this is sometimes applied to have the fact that you're just putting the body in such an insulin state of constantly pumping out insulin. Even if your cells are sensitive to that effect now, or more sensitive than they might be on a higher fat diet, I'm worried about how much insulin you are producing with such a high carb diet. That's, I guess my hesitation with that.
I have not seen it work that well., but here is the thing, it's crazy how personalized everyone is. There's absolutely no one size fits all. I would say in my people that are showing signs of insulin resistance, which in the general population is 80% to 90% of the population has some form of metabolic dysfunction. They tend to do best on the lower carb diet. This doesn't mean it has to be zero carb, this doesn't mean it has to be keto, but they tend to do better on a lower carb diet, but then there's this subset of the population that just doesn't, and they do better on a lower fat, higher carb diet. I would say as a general rule of thumb, I see much more success with the lower carb, but there's always people who don't do as well.
There's that really famous study where it was like a one of the best design diet studies, where it's 12 months long, and it was high carb versus high fat. Essentially, what it showed is that overall, there wasn't a lot of significant differences, but that there was a ton of inter individuality. Essentially, what that says to me is there's this group of people who respond really well to one, and then there's a subset of that that doesn't. You really have to figure out an experiment what one is going to work best for you because it's not as simple as everyone needs to follow keto, or everyone needs to follow low fat, high carb. I think the low fat, high carb subjectively is a little bit harder to stick to because the fat criteria is just so low that it's hard for people to stick to that. I've just seen it, it's more difficult to do it in the long term as well. You also want to find something that's sustainable for you and works for you. It's not just something you're going to jump to a diet for two weeks and then jump to something else.
I really want to find something that works for somebody with their physiology, with their genetics, epigenetics, all these things that make us unique, but also something that they're not going to crash off of and have a rebound in standard American diet. So, that's the worst diet for everybody is the standard American diet. I want to make sure that we're picking something that is sustainable as well. And I do worry about that.
Melanie Avalon: I love your approach to all of this so much. Everything you said is exactly how I feel. I mean, it's crazy how different we all are and how it is so individual, and it bothers me that people try to often prescribe one diet to everybody. I keep saying, if there was one diet that worked for everybody, I think we would have found it, because I think we would all be doing it.
Kara Collier: There won’t to be so much controversy in nutrition if there was one answer. There's not one cause of insulin resistant, there's not one solution, there's not one diet. We can all do better by eating more whole foods and avoiding anything processed. That's like, obviously a good general rule of thumb, but beyond that, it is super, super individual.
Melanie Avalon: So, speaking to that the timeline of all of this. Let’s say a person actually is in a state of physiological insulin resistance, and they want to bring back the carbs. Does it vary by individuals as to how long it takes their body to make those changes? Or, on the flip side, really switching between any type of macros, is it usually a few days, weeks, individual?
Kara Collier: It does vary. I would say as a general rule of thumb, it can be pretty quick. This has been studied in regards to like a failing an oral glucose tolerance test. Pregnant women, they have to take an oral glucose tolerance test to make sure they don't have gestational diabetes, and that's when this was first observed was people who were following a really low carbohydrate diet, they would fail these tests, because all of a sudden, you're having to drink 75 grams of pure glucose and your system hasn't seen glucose, and you have this massive glucose response, and you're labeled as gestational diabetic. When really, it's just physiological insulin resistance.
What they've shown at least with these gestational diabetes false alarms is about three days or so of eating 100 to 250 grams of carbohydrates per day, is enough to make that effect go away. And then you can retest, and the results come back normal. For most people, if you're eating enough carbs, you might see some higher responses in those couple days. So, if you want to avoid spikes at the same time, it might take longer, because we'd have to gradually work our way up there. But if you're okay with three or four days of high numbers, because you're really upping your carbs, all of a sudden, it should reverse fairly quickly at that point.
Melanie Avalon: Actually, Rachel had a question about those tests. She said, “Can the glucose monitor be used during pregnancy to avoid the icky glucose drink? Could this be a better option for low carb moms? Can MDs petition insurance companies with this rationale?
Kara Collier: Yeah. We get this question a lot, and I do find it really interesting because essentially, an oral glucose tolerance test, you're just having to drink this pure glucose, and I'm not sure if you've ever had one, but it isn't very fun, especially if you're not normally consuming carbohydrates, but they're doing it to test your insulin sensitivity. And that postprandial response to a big glucose load is actually extremely interesting. It tells us a lot about how your body can handle glucose, but I definitely understand that if you're not eating carbohydrates, you really don't want to do this test. I think a CGM could be an alternative because we can see these nuances and your data and get an understanding of if it looks healthy or not.
It would be whether we can convince official medical boards to accept this as a diagnostic criteria. I have a feeling that's going to be really hard to do because something like an OGTT, take the test and we're looking at very specific things. How high did your glucose go? What was it at two hours? It's easy for an MD to assess, yes or no, abnormal, not abnormal, where if we just put a CGM on somebody and were like, “Go live your normal life for two weeks and then we'll look at your results.” That require somebody to really specialize in interpreting and understanding like the daily nuances and CGM data, and I just have a feeling that that won't be part of like a standard diagnostic panel because it just doesn't seem realistic. I think it would be a good idea. We do have some people who have a functional MD or a midwife, and they're okay with using the CGM and replacement of this, but it's certainly not standard or recommended in mainstream medicine.
Melanie Avalon: Do you have any idea why with the physiological insulin resistance that occurs on purpose during pregnancy? Why some women, it does reach dangerous levels and potentially can make them prediabetic or have issues with diabetes later, and some women are fine? Do you think it's a matter of just personal biology or diet during pregnancy? I just don't know if you have any thoughts on all of that.
Kara Collier: Yeah, that's a good question. Pregnancy, it does put you in a state of mild insulin resistance, where you're not as glucose tolerance as maybe when you weren't pregnant. But then, there's the next level of showing signs of gestational diabetes, which would be even higher levels and just baseline what pregnancy puts you in. I think that that really comes out during pregnancy, because you're in this state of physiological insulin resistance. So, it amplifies a problem you might have. If you're showing really mild signs of insulin resistance, that cannot be detected on something like a fasting glucose or an A1c, because you're not seeing the nuances like you might see on a CGM data. I think that just becomes amplified and much more clear when you're in this state of physiological insulin resistance during pregnancy. So, people who might be having issues before, or they might have a poor diet, but they kind of got away with it because their system was functioning a little bit more appropriately. When they become pregnant, they can't really get away with it anymore because we're just in this altered state of glucose metabolism.
Melanie Avalon: Reading Dr. Bikman’s book, he’s saying that breastfeeding is actually one of the mechanisms that reverses the insulin resistance. I found that so fascinating. Do you know why?
Kara Collier: I don't know why. I haven't personally looked into that that much, but I do know that glucose levels-- because we see a lot of moms postpartum and glucose levels dip during breastfeeding because it's like a workout. You're burning calories, your body is in a high metabolic demand. So, that's my hypothesis is that you're really just burning extra calories, higher basal metabolic rates. It's like you went out for a run or you went to the gym during that time. And if you're doing it every two hours all day long, it's like you're moving and you're active all day long, which we're not always in modern society.
Melanie Avalon: Gotcha. We keep talking about HbA1c, is it a half-life? Or is it just a three-month reflection of cells?
Kara Collier: Yeah, it's a three-month reflection. We were talking about that glycation, so it's essentially saying how much sugar is attached to your hemoglobin molecules. And the hemoglobin lasts for about 90 days, so three months. So, it's telling you on average, what have your average circulating glucose values been in the past three months.
Melanie Avalon: So, if a person is standing here right now and they get tested, three months from now-- so, if you will make dietary changes in three months, you should be able to see a complete change? Because in theory, then wouldn't you be able to drop from the highest of high to zero in three months?
Kara Collier: Theoretically, your A1c will probably never go below like 4. There's always a baseline level of glucose in the system because we need glucose to live. Our glucose is never zero. So, if it was zero, you probably wouldn't be alive.
Melanie Avalon: Okay, so drop to 4.
Kara Collier: Yeah. Theoretically, if you made very intense lifestyle changes, you should be able to see a drop if you rechecked it three months later, at least some sort of decrease.
Melanie Avalon: Do you have thoughts about fructosamine? I've often heard that that's a pretty telling thing that people don't often measure, but you could measure it.
Kara Collier: I do, and I have thoughts on A1c too. With the hemoglobin A1c, it's not my favorite test. I feel it has been dubbed as the best test to see if what your glucose is doing, and if you're diabetic or not, but it has a lot of problems. One inherently is that it's telling you your average glucose, which is useful, it's interesting to know how much glucose is circulating at all times, but it's missing the variability which is actually more of a telling signal of how things are going. So, it's not telling you if your glucose is spiking to 200 and crashing to 60 all day long or if your glucose is right at 120 all day, those two could be the same A1c because we're only taking the average. So, I do think in that regard, it needs to be taken with a grain of salt. But also, it tends to be pretty unreliable, again, it's making that assumption that a red blood cell, which has the hemoglobin lasts for 90 days, but there are a lot of situations and conditions that alter our red blood cell life. Anemia, which is very common, is going to alter how long your red blood cell lives. Even a low carb ketogenic diet alters your red blood cells, blood loss, smoking, vitamin B12 deficiency. All of these things alter your red blood cell, and it can skew the result either a little bit higher or lower than true value.
This has been studied, and it tends to only have on average about a 50% sensitivity. So, only about 50% of the time, is it truly matching with your average glucose values when they're measuring it with more sophisticated, like clinical research measures. So, for that reason, if you come back right on the bubble, if you're generally healthy, normal A1c is considered below 5.7. So, if you're A1c is 5.8%, that's technically prediabetes, but you do a lot of things right, then I'm going to take that with a grain of salt, and I want to see CGM data, I want to see all these other metrics that assess metabolic health because it could just be a false negative, and it could just say, like maybe you have anemia, or maybe you're following a ketogenic diet.
What I think A1c is useful for is, if it's majorly high, so if your A1c is 10%, there's no amount of anemia that's correcting for that. So, 10% is really, really high that tells us something, but I also think it's really useful for tracking personal progress. If your A1c was 8% last year and you've retested it, and now it's 6%, that is your personal progress, you can clearly see a downward trend, that is still a very useful insight, even if the absolute numbers may be skewed higher or lower. So, I guess that's my caveat with A1c.
Melanie Avalon: Quick question about that. I'm assuming with a low carb diet, there's the potential that the blood cells would be living longer so you might see higher HbA1c. For anemia, wouldn't they be dying sooner so you might see a lower HbA1c when really--
Kara Collier: Exactly.
Melanie Avalon: Of course, in anemia, they might think their A1c is fine, but there actually might be problems because the blood cells are--
Kara Collier: That's exactly right. Yeah. It can be both directions where maybe you think your A1c is telling you you're prediabetic, but you're fine. Or you could think, “I'm good to go,” but it's actually in prediabetic levels. So, yeah, it can be both directions depending on the situation.
Melanie Avalon: Wow. Yeah. So, the fructosamine, what is that looking at?
Kara Collier: Yeah, so fructosamine is also looking at average glucose based off of a glycated protein, but it's measuring it on albumin rather than hemoglobin. And that has a much shorter half-life, so it turns over in two weeks. Fructosamine is instead telling you what your average glucose values were in the last two weeks. So, this is really helpful. Traditionally, it's only used if you're making medication adjustments for diabetics type 1 or type 2. If you make an adjustment and insulin dosage, and then two weeks later, you can test it with a fructosamine rather than having to wait three months to make a medication adjustment. So, that's the standard use case. But essentially, it's telling us in a much shorter time how things are changing, and it's more reliable because it is measuring albumin, not the red blood cells. So, if you do have abnormal red blood cell length, then fructosamine is a more reliable choice and you won't get as many false highs or false lows. Albumin can also vary. So, it is usually low with things like renal issues or hepatic issues. It's not something maybe the biohacker crowd has to be too worried about, but there are instances where albumin can also be falsely low, chronic inflammation in general, can lower albumin.
Melanie Avalon: Does dietary protein affect that at all?
Kara Collier: It doesn't. We used to think that it did. When people came back with a low albumin, we used to amp up their protein in the hospitals, but, no, it's more reflective of inflammation and what's going on with different organ systems rather than any dietary reflection.
Melanie Avalon: I love this so much. I got a lot of questions about a pattern which-- this was actually a pattern I was anticipating before I ever put on the CGM. I was like, “I'm calling it.” I was like, I think I'm going to see in myself like higher blood sugar levels while fasting and then I feel like when I eat, it's probably going to go down. Maybe like a reactive hypoglycemia or reverse pattern. Mercedes says, “What to look out for if I'm reactive hypoglycemic?” Sharon, she says, “I've been using one for two weeks, and I found that my glucose goes down sharply to 65 when I eat and crashes at points when I'm sleeping. To make things crazier, it runs high, not out of range 105 to 116 when I fast. Could you ask what it means when you seem to be the opposite and punch downward after eating and up when fasted?” Is that a common pattern for people?
Kara Collier: Yeah. There are two different categories of hypoglycemia. So, there can be reactive or functional, which is typically after a meal. And then we can have fasting hypoglycemia, which is usually occurs when you're sleeping. The most common cause of reactive hypoglycemia is usually if you're consuming, like really refined carbohydrates, or sugar. So, this is the most typical scenario where somebody eats, who knows what, maybe a soda, and you pump out a bunch of insulin to correct that high glucose and your body basically, like, overestimates how much insulin it needs. So, you release a bunch of insulin, and then your blood sugar crashes because of that huge insulin dump. And then your body tries to bring it back up. And then you have these fluctuating glucose levels as your body tries to fix what's going on. And this can feel really, really awful for a lot of people.
So, if this is going on, we really want to monitor what type of carbohydrates are choosing and how many you're eating at any given point in time because this is definitely a problem. And this is a really, really early sign of a potential problem. If you eat something minor, maybe a plain sweet potato and your glucose spikes, but then crashes hard, and you feel those feelings of dizziness, nausea, anxiety, sweating, mood swings, that might be a sign that your body is putting out too much insulin every time you're eating, and we want to work on that. So, that's the most common reason.
I will say that some people, especially people following a ketogenic diet, or really low carb diet, their glucose might decrease after meals, but it's not this huge spike and drop. It's just maybe you started at 110 when you ate the meal and your glucose went to 90 and you decrease, but you're not getting to a level where you're feeling hypoglycemic. So, you're not having those symptoms, and that's normal. A lot of times, especially if you're stimulating ketones, or if you're eating a lot of protein, you might be also stimulating a little glucagon with that. Your glucose can decrease a little, so that is not hypoglycemia. That might just be a small glucose decrease after a meal.
Other causes, potential causes of hypoglycemia, especially reactive hypoglycemia is if you're somebody who maybe has hypocortisolism, so lack of glucocorticoids from the adrenal glands can increase glucose oxidation and decrease gluconeogenesis. So, people who have maybe, I guess, it's a little debated, but what I would call, I guess, cortisol issues. If you're having a lot of stress, we see some reactive hypoglycemia for this reason. And same with, if you're having, maybe thyroid issues. So, like hypothyroidism, can also cause hypoglycemia. These are two medical conditions we want to check for. And if you have either of those, then that's a medical problem you need to take to your doctor and the side effect of that is potential hypoglycemia. Once we fix that, we can fix the hypoglycemia. There could be a lot of things going on.
Also, many medications can make people hypoglycemic in the middle of the night. We also want to know what they might be taking. For some people, some very common antibiotics can cause hypoglycemia. ACE inhibitors, like bile acid sequestrants, beta blockers, some pretty common medications, of course, diabetic medications, but these can also cause hypoglycemia. Also, if you're consuming alcohol, at meals or on its own, this can cause hypoglycemia for a lot of people, especially the nocturnal hypoglycemia. Essentially, the alcohol is interfering with the glucose homeostasis because the liver is prioritizing alcohol detoxification. Some people see this effect more intensely than others do, so this is something else where I have had clients where just one glass of wine at night causes them to dip in the middle of the night. So, not everybody sees this, but that's something else we might want to look for in these scenarios.
Melanie Avalon: You're talking about with people who are stressed, the cortisol issues, does the situation look does their blood glucose raised from the stress and then the responses it drops, so it's a reactive hypoglycemia to themselves?
Kara Collier: Yeah. We can see in both scenarios with that issue of. It could be the fasting hypoglycemia or the reactive. Reactive is often associated with the content of your meal itself, and potentially this problem of excreting too much insulin, but sometimes we see it where-- we've looked at the meals, the meals look good, it doesn't seem to be what's going on. It's actually a cortisol issue that's interfering with metabolism, and so that can be a whole separate problem. Then we probably have to address that, bring that data to your doctor and talk that through, but that has happened many times.
Melanie Avalon: So, it's in the context of eating, not the fasting, or it does happen in the fasting as well?
Kara Collier: Yeah, it can happen in either.
Melanie Avalon: Okay, that's fascinating. I have a super random question. This is so random, because a lot of people, me and my audience, often have digestive distress and will use things digestive enzymes. Have you seen anything where using too many sort of digestive enzymes can make your food potentially more refined or processed in a way, so it has a bigger effect on your blood sugar? If people are eating fruit and they're taking a lot of digestive enzymes with it, would that potentially make it more sugary then?
Kara Collier: No, I see what you're saying. I'm not sure. This would be something I'd be very curious to have somebody try out. So, if you want to do a little [unintelligible [01:16:53] experiment, I would be super interested. If you see different responses, if you take it with a lot of enzymes versus maybe none or small amount. I mean, theoretically, you could be essentially processing the food more. We do definitely see different glucose responses depending on how processed the food is. Example of whole fruit versus juice or Steel-Cut oats versus Instant Oats, the effects are pretty dramatic in glucose responses to just the form the food isn't. I think in theory, it could potentially have a higher glucose response if you're making it essentially more refined. But I'm not sure if it would actually play out that way or not. It might not. I haven't had anyone tell me that or notice that if it is.
Melanie Avalon: These are the things I think about. I mean, I've definitely noticed not to go into TMI territory, but a very definite change and stool consistency with enzymes. To me that says, well, there's a lot more processing going on in one situation and not the other, so I've just been thinking about that. Another timeline question, the FreeStyle Libre and Nutrisense, it's a two-week period, like we've been saying. I got a lot of questions about what you can learn in those two weeks, and how long you need to be using one. Margaret said, “Is two weeks really long enough to get a clear picture of your glucose levels, and how different foods or activities affect your glucose levels is a month better?” Andy says, “Is a two-week monitoring period a good enough snapshot? Would you recommend varying eating patterns, diet, sleep, exercise, and alcohol consumption while wearing a monitor?” We haven't aired this episode yet, obviously, but I have been teasing it and given the code in my Facebook group to my audience, and I'm getting so many questions about, should I do a two-week trial? Should I go ahead and do a month? Should I do a year? Because you guys do offer a lot of different plans for that. People with those questions, what do you recommend? Oh, and do you wear one 24/7?
Kara Collier: I don't wear one 24/7 anymore. I would say for me the first-- I did three months of back to back wearing and an experimentation as much as possible. And now my sweet spot after that is wearing one maybe every six weeks. I did this back to back have a few months to just learn as much as possible. And then I like to check it in to tweak or if I have an experiment I want to try or to just keep myself accountable. One of the amazing benefits of these devices is, it really drives behavior change. So, if somebody that has a hard time sticking to your plan or sticking to the things you know you should do, but they're hard to do sometimes. Having that real-time data is super helpful to just motivate you to do the certain things. You don't forget that that data is there. So, I find it super helpful to just check in and get myself back on track if I need that. That's my personal usage.
Melanie Avalon: There's a two-week trial. What are the different tiers? And then is it three months, six months, a year?
Kara Collier: Essentially what we offer is we have the two-week trial, which is just one CGM. You get the app and the dietician, you get everything, but there's no commitment, you don't have to do anything else after that. I think the two-week plan is a really great option, if you're not sure if you're going to like it or not. So, it's basically if you're afraid of committing, but you think you might want to do it longer, you could start with a two week and then no harm, no foul if you just didn't really like wearing it, or you felt like you got enough information from it. So, it's a good place to start if you're not sure.
It's also a good place if you are pretty routine driven. Let's say you follow ketogenic diet, you like what you're doing, and you just want to see like, where am I glucose levels at? Is everything good just to check in? Two weeks is enough time. Whereas let's say you're trying different diets, you're like, I want to see if keto works. I want to see if a higher carb works, or I want to try different fasting regimens, that's going to take longer than two weeks if you have a bunch of things you want to try out and experiment with. I think it depends on your goal. If you have bigger goals as well, where it's like you maybe really want to lose weight, or you want to get your glucose values down, maybe you already know they're in pre-diabetic levels, or you have these bigger picture goals, it takes more than two weeks to realistically make progress on those things. We do offer monthly options as well.
We have a month to month, again, for the commitment-phobic people out there where you could cancel it anytime. Obviously, it's a little bit more expensive, because you're not committing at all. But that's an option if you thought maybe I want to do a month, and then you could switch plans if you feel you'd like it. And then we have 3 months, 6 months, 12 months, and then it just keeps getting cheaper the longer you commit. For the longer plans, if you know, I have 30 pounds, I want to lose or I'm pre-diabetic, or I know I want to try like a couple different diets and experiment, I think three months is a good option.
Melanie Avalon: Listeners, so speaking from my experience, because I didn't know what to expect going into all of this. If you're the type of person where this content is really resonating with you, and you want to explore and learn and are anticipating making dietary changes, I feel most of you guys will probably-- two weeks will go by and you will be like, “I wanted to go a little bit longer.” Like she said, just doing a checkup, see where things are, the two weeks would completely work. For me, I think I probably will do it, I don't know, anticipating probably about three months or so and then do the checkups. I can say this again later, but we do have a discount for you listeners, which I'm so grateful for. So, if you go to melanieavalon.com/nutrisensecgm, you can use the coupon code, MelanieAvalon, and that will get you 15% off everything, except not the two week one, but everything else it should apply for. So, thank you so much for that, by the way.
Kara Collier: Yeah, absolutely. One thing I will note too, if you do our monthly plans, you can pause your plan if you ever want to. So, if you want to take a month or two-month break, you can pause, so it's flexible if f you need to spread maybe a couple months out over some time.
Melanie Avalon: Is that on a different page? I didn't see that-- I need to find the link to that because I didn't realize that was an option. I think I just saw the page for three, six.
Kara Collier: Yeah. Basically, if you sign up for any of those, you can just send us a message and say like, “Oh, I want to pause my account.” We can pause it for a certain amount of time and just work with you on what's best. I can send you information on that, but it is flexible if anyone ever wants to take a break, we can definitely do that.
Melanie Avalon: Awesome. And then the actual Nutrisense app itself. I got a lot of questions about interpreting the data because a lot of people in my group actually said they did have access to a FreeStyle Libre through their doctor, and they were wanting to know what was the difference of having the nuisance app. Sue, for example, says, can she get a how-to interpret readings. Derrida says, “What do you do with the data? Can an average person interpret the data?” Ingrid says, “How to interpret results to figure out what works for the individual and which foods don't work?” The actual Nutrisense-- so to clarify for listeners, the FreeStyle Libre is the actual CGM device. Nutrisense is the company, the app that is providing the prescription, the access to the CGM, and then their app syncs with your device and has a ton of information that you can learn about yourself. So, using the app, what will listeners learn? How does it work? How does it work with the coaching or the communicating with the nutritionist? What's going on?
Kara Collier: There's two components. If you were just to get the FreeStyle Libre from your doctor and use the app that comes with it, there's two things that really differentiate our product that we're trying to fill the gaps that currently exist in. One is build an app that is geared towards the nondiabetic and the person who wants to understand their data. So, if you use the Libre app or the Dexcom app, they're built for diabetics. So, it basically tells you your glucose values and it tells you, as you enter how much insulin you're taking, so that you can manage your glucose with medications. And that's about it.
We're trying to build an app that helps the person who doesn't necessarily have diabetes and is really focused on these other goals make use of this data. We have, of course, statistics and charts to help you understand your data, but we also have a food tracker. So, you can see, match what you're eating against your glucose. We have integration with other metrics. So, you can utilize and monitor your ketones against your glucose. And that's one of our big picture goals down the road is to keep integrating with other data that gives you a good holistic view of your metabolic health. Ketones and direct-to-consumer labs that you can order from the app, and then the information is there. Integrations like that, with Oura Ring and all these other trackers.
But the real differentiator, I think, is the dietician support. Of course, I'm a little biased because I am a dietitian, but we provide a one-on-one dietitian for each customer. We do this for multiple reasons. One is because as it was probably made clear today, glucose can be confusing, and it can be nuanced. There are many reasons your glucose might increase or decrease. A lot of questions come up and we want to make sure that you're getting the most out of the information and that you're actually able to reach your health goals. We don't want to just sell you a product because it sounds interesting, we actually want you to be able to improve and optimize your life. Sometimes, a human touch is needed for that. We have a trained dietician who can work with you that are all trained and understanding glucose values, optimizing metabolic health, and they're there to help, answer your questions, but also help point out things in your data so you understand it, suggest experiments based off of your individual goals, and really help provide that personalized experience because at the end of the day we truly believe there's not one size fits all, and everyone's unique. You need a human there to help you find the right thing for you.
The dietitian is included for everybody because a lot of people think they don't want a dietician because they think a dietitian is going to put them on a diet. But that's not what our dietitians are there for you. They're there to really make you a glucose expert and to totally understand and optimize your data, and also help you reach whatever your unique health goal is. So, it's very personalized, and it's basically like texting for the customer. It all happens through the in-app chat. It's right there in the app that you can send a message anytime you're confused, and you're always getting feedback from that coach.
Melanie Avalon: Yeah, I will say I was ridiculously impressed with that aspect of it. I as well did not anticipate-- like you said, people think, “Oh, I don't need to talk to a dietician.” But the communication has just been so-- I mean, I don't know if I can say names. I've been talking with Carly, and she's just been amazing, and has answered all my questions. It's really nice to have somebody there. But at the same time, she's also said, “If you prefer not to have-- be communicating or us looking it over, just let me know.” It's really what you want to make of it. It's been really, really valuable. And Nat wants to know, “Do you ship overseas?”
Kara Collier: Right now, we only ship to the US and Canada, but we do have many people in other countries who are using our app and dietitian, but they're getting the sensors over the counter. We have a lot of people in Europe where they can just walk to their local pharmacy and get the Libre device and then maybe they've tried it on their own and they needed help understanding the data or they wanted a better app, and so they ended up reaching out to us. Now, we offer that as an option for international customers if they're able to get the Libre or if you have a Dexcom and you have an iPhone, we also are compatible with the Dexcom. If you can get your own sensor, then you can definitely use our app and use our dieticians.
Melanie Avalon: Okay, yeah, because Miranda, she says, “Well, they have a software-only package for those of us already using a CGM.” So, is that on the website, or do they need to contact?
Kara Collier: It's not on the website at this point, because it's something that people have just been reaching out to us about and so, we're starting to do, but it's not one of our official plans at this point in time. You can just send us a message. We have a chatbot on our website, and somebody will be able to send you pricing and set you up with that. We can have an option where if you're just using our app, or if you want to use the app and the dietician, we can definitely do both of those.
Melanie Avalon: Okay, awesome. Do you know much about the EMF exposure of wearing a CGM? I know that's a big concern.
Kara Collier: This has been very lightly studied. I will say the research is not in-depth. But it has shown that it's essentially minimal to none because we're actually using the NFC, like near field communication, in your phone. It's a chip in your phone that reads when you do Apple Pay or Google Pay, that's how that works. And so, that's what you're using to scan the device. Whereas something like Dexcom, or there's a different version of the Libre that uses Bluetooth, and that has a higher EMF output because it's using Bluetooth and it's constantly pulling signals from the device. So, that's one benefit. It's a double-edged sword where you have to manually scan the device rather than Bluetooth just automatically synching it, but it has lower EMF. So, I think it's kind of a whim.
Melanie Avalon: Actually, do you think in the future, they'll probably all move towards Bluetooth?
Kara Collier: Probably. Yeah, it's probably inevitable. I have no idea, but I'm assuming, yes.
Melanie Avalon: Yeah. I will say one thing I learned, for listeners, is if you put your phone into airplane mode in the middle of the night, using the app, and this might be a fix that will be updated when this comes out, but it'll scan, but it doesn't actually scan because I didn't say this yet on the show-- We didn't say this yet, but you do have to scan it. If you want 24 hours of data, you have to scan it at least every eight hours. If for whatever reason you're waking up in the middle of the night, listeners, you briefly turn your phone off of airplane mode just to scan it. I had about three days where I was like, “I don't think it's getting any of my data at night.” And then, we figured out it was because of the airplane mode. It would vibrate like it had scan, so I just assumed it was scanning, but alas, it was not.
Okay, this has been absolutely amazing. I just want to thank you so much for all that you're doing. Literally, this is my new obsession, CGMs and everything that you're doing with this company, making it available to everybody is just so valuable. Listeners, I cannot recommend enough at the very least doing a two-week trial and just getting a clear picture of everything. What are you most excited about with the future of this company?
Kara Collier: That's a good question. I'm really excited about the other integration. I think glucose is so interesting and so important, but we really do want to eventually be a company that's really looking at a holistic view of your metabolic health. Right now, if anybody has labs, they can send it to us and we can take that into account, and it gives us a better view of what's going on. But eventually, we want you to be able to upload the labs you have into the app and it's very organized and tells you a lot of information and tracks and gives you trends not just on glucose, but these other metrics that are so important because really, our ultimate goal is to just make you the healthiest version of yourself. We do want to incorporate other wearables, other integrations, lab data so that we can get this well-rounded, 360 view. So, that's what I'm excited about.
Melanie Avalon: I love that. I've heard that-- do you know if there's a future of something that doesn't even go in your skin?
Kara Collier: Yeah, they definitely have been testing out all types of devices. So, it will be interesting to see where the actual hardware goes. I do think they're also going to just keep getting cheaper and cheaper because there's so much more interest in this. So, that's also exciting that I'm looking forward to. But, yeah, there is some companies trying to develop something where maybe it measures it more of your sweat or the surface of your skin. So, it's not actually inserted anywhere. And then, there's also companies going the opposite direction where it's actually surgically implanted, but it would last longer, it'd be three months of data as opposed to two weeks. So, I'm sure we'll see all types of things coming up, which will be super interesting.
Melanie Avalon: Awesome, so many exciting things. Well, the very last question that I ask every single guest on this podcast comes from my growing realization each and every day, just how important mindset is surrounding everything. What is something that you're grateful for?
Kara Collier: I love that question. I feel it sounds cheesy, but the first thing that comes to my mind is I'm just definitely grateful for our customers. I think coming from-- usually you get into healthcare because you want to help people and then working in the hospital where everyone's sick and sad, it's just frustrating. Every day I get to work with people who are so excited to be their best version of themselves, and it's so inspiring. Sometimes, people have more work to be done than others, but the level of motivation and invigoration that our customers have to just be optimal and take it to the next level is really inspiring. I'm very excited about the wave that we're having with health and people caring about their bodies and caring about what they're putting in it. I'm grateful to work with those types of customers every day.
Melanie Avalon: I love that so much. It's so wonderful when people are doing such amazing things like this, and then loving what you're doing, loving the people you're working with. And it's having massive effects on people's health and vitality. So, I cannot thank you enough. Listeners, the show notes for today's episode, there will be a full transcript and we'll put links to everything, that will be at melanieavalon.com/nutrisense. Like I said, for a discount, just go to melanieavalon.com/nutrisensecgm and use the coupon code, MelanieAvalon to get 15% off. Any other links, resources, Kara, that you like to put out there for how can listeners best follow your work?
Kara Collier: Yeah. Our Instagram account through Nutrisense, we're definitely putting out any interesting research or things we're learning is going through there. Of course, our website. We're also putting out blogs. So, many of the Nutrisense accounts are the best way to see my voice through that. I would say I don't do a great job of keeping up with my own social media. It's hard when you're also trying to build a company, but a lot of my thoughts and things I'm interested in are coming out through the Nutrisense accounts.
Melanie Avalon: Awesome. I love it so much. I will put links to all of that in the show notes. And this has been absolutely fabulous. Thank you so much for what you're doing. Hopefully, we can stay in touch and talk again in the future.
Kara Collier: Yeah, absolutely. Thank you so much for having me.
Melanie Avalon: Bye.